
Tiny Models, Big Impact
Organoids are reshaping cancer R&D by providing more accurate, patient-relevant models than classical methods. By bridging the gap between preclinical and early clinical stages, they enable patient-centric target validation, drug discovery, and therapeutic development, representing a significant step toward truly precision oncology
Human-like, three-dimensional Cancer Models
Organoids – three-dimensional cell cultures that more accurately mimic human normal and tumor tissues – have become a transformative tool in cancer research. Unlike two-dimensional cell cultures, organoids can better preserve the cellular diversity and heterogeneity of the original tumor. They are mechanistically superior to 2D cell lines, because their structure preserves the architecture, polarity, spatial organization, and many gene and protein expression features of the originating tissue. Moreover, organoids can preserve tumor architecture and cancer-cell-intrinsic features. They can model certain cell–cell interactions when co-cultured with stromal or immune components.
By thus replicating the complexity of human tissues, organoids exhibit physiological responses to treatments under near-in vivo conditions, enabling patient-specific target evaluation, drug screening, and therapy evaluation. This makes them powerful models for studying disease mechanisms, cellular interactions, and tumor progression.
Applications in Oncology Research
Organoids are increasingly being used in cancer research. For example, in the context of colon cancers, where tumors are classified into four consensus molecular subtypes with distinct biological behaviors, prognostic profiles, and therapeutic responses – typically determined through complex gene-expression analyses – organoids can capture these subtype-specific features and facilitate more physiologically relevant studies. Building on this, a recent publication describes the generation of colorectal cancer organoids that retain the APC-KRAS-TP53 mutational landscape. By applying advanced data techniques to identify patterns in alternative splicing and their connection to cancer subtypes, a subtype identifier model could be created that more accurately classifies tumors, making the new protocol suitable for clinical applications. Additionally, the organoid-based model may provide additional insights into the cancer cell features compared to tissue analysis due to the enrichment for cancer cells relative to stromal components.
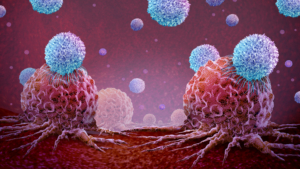
Other projects study the interaction between immune cells and tumoroids, exploring how to “train” T-cells to recognize and attack cancer cells, potentially overcoming tumor evasion mechanisms. These co-culture systems allow researchers to investigate patient-specific immune responses and evaluate novel immunotherapies in a controlled, physiologically relevant environment with heterogenous cancer cell populations present in a tissue sample.
These advances offer hope that organoid technology could play a transformative role in developing personalized immunotherapies and more effective cancer treatments in the near future.
Turning Data into Personalized Oncology Treatments
However, standardization is key when preparing organoids, as even organoids from the same patient can yield divergent results due to variations in tissue processing and culture conditions. Adding to this complexity is the profound heterogeneity of tumors, both within individual patients and across populations. Also, batch variability and protocol heterogeneity can limit regulatory acceptance and cross-site comparability.
To unlock the full potential of organoids, reproducible, robust, and well-characterized workflows are therefore indispensable. Emerging organoid biobanks and standardized QC pipelines are just beginning to address these issues.
A deep molecular profiling of the patient tissue, coupled with patient-derived cell models generated from the same patient, enables a truly data-driven approach that remains patient-centric from the outset of discovery through to development. This integrated strategy is essential not only for accurate target identification across tissue types and patient subgroups, but also for mitigating translational risks in preclinical and clinical development.
Towards Patient-Centric Approaches
The spatial information that organoids retain can provide mechanistic insights and functional validation in a human setting. Compared to conventional cell cultures and animal models, they can be used to reveal signs of drug resistance more efficiently, reducing translational risk. Also, data from organoid experiments can inform clinical trial design and support patient stratification by predicting responder/non-responder patients and optimizing inclusion criteria.
Forming a bridge between the preclinical and early clinical stages, organoids are paving the way for more effective and personalized cancer therapies. They support the identification and validation of new therapeutic targets and biomarkers, as well as the development of new treatments and companion diagnostics.
To fully realize this potential, standardized protocols, robust quality control, and integration with molecular data are essential. As these frameworks mature, organoids will increasingly inform translational research and clinical decision-making, helping to bridge the gap between preclinical studies and individualized cancer care.
This article of Dr Parvaneh Mohammadi, Director Primary Cell Modelling, Indivumed, was originally published in the Q4-25 issue of the |transkript magazine (German-language).


 Roche
Roche
 freshidea / Adobe Stock
freshidea / Adobe Stock