Sepsis: Targeting a silent killer
For over three decades, attempts among drug developers to target the inflammatory pathways and symptoms of sepsis have been fruitless. New rapid diagnostics, rigourous patient stratification and drugs with novel modes of action are now on the horizon for treating the most costly cause of death in the industrialised world. Biotechs are pushing new ideas towards clinical testing, but there just isn't enough funding available in the EU. Will US investors again pick up European innovation on the cheap?
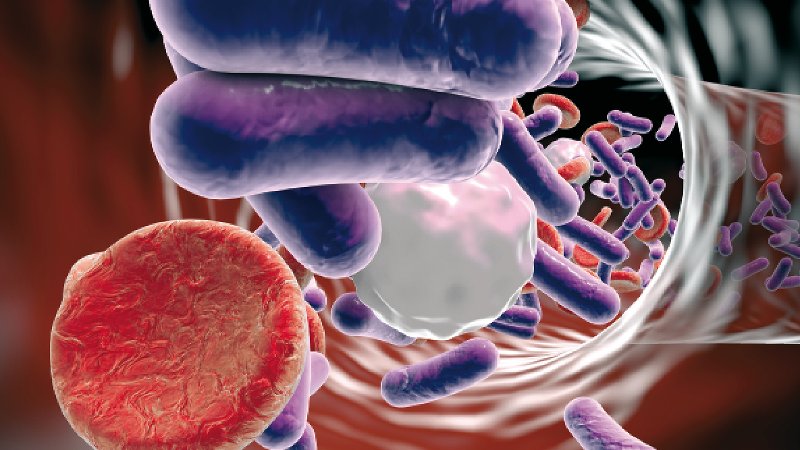
Sepsis is a life-threatening condition that arises when the body’s response to an infection injures its own tissues and organs. It occurs when the body’s local response to an invasion and microbial toxins – in Ali’s case a respiratory infection – expands to the entire body. The condition is a ruthless, silent killer.
Somewhere in the world, someone dies of it around every four seconds. In the nations of the South, collateral damage caused by the systemic infection is greatest. Every year, six million babies and 100,000 mothers from the poorest part of the world die from sepsis, in the throes of symptoms that include uncontrolled inflammation, vascular leakage, severe hypotension, organ damage and shock. It’s the most common cause of death by infection there. But even in countries with well-equipped ICUs such as the US, about 260,000 of the 1.1 million patients who are diagnosed with sepsis each year die. With annual costs estimated at US$24bn in 2013 – US$3.4bn more that two years before – sepsis therapy and post-treatment eat up a whopping 7% of the US healthcare budget. In Europe, which counts 1.2 million sepsis infections each year, the situation is no better. Around 40% of all ICU patients die from the amok immune response.
Due to its complex etiology, there is still not a single drug approved for market that could stop the condition’s inexorable march. Since the 1980s, drug developers have carried out more than 60 late-stage clinical trails with sepsis drugs that target the molecules triggering host response, but most failed to improve patient outcomes.
Read the full background on sepsis in our print magazine!
- How sepsis and septic shock develop
- Current standard of care
- New tests and biomarkers for early diagnosis
- Novel European approaches
- Outlook and expert opinion



 adobe.stock.com - ipopba
adobe.stock.com - ipopba BioDlink
BioDlink