Newron secured €38m to test a potential new class in schizophrenia
Newron Pharmaceuticals has secured up to €38mn to advance Phase III trials of evenamide, a drug that, if successful, could represent one of the first circuit-modulating therapies in schizophrenia.
The agreement provides €15m upfront, with a further €11m linked to development milestones and €12m payable if the pivotal ENIGMA-TRS trials deliver positive results. The staged financing is designed to carry the company through a decisive 12-week Phase III readout expected in late 2026. “This financing is expected to extend our operational runway well beyond the upcoming 12-week results from the ENIGMA-TRS 1 and 2 pivotal studies and support continued execution of our Phase III development program,” said Roberto Galli, Newron’s chief financial officer in a press release.
The capital raise is also a bet on a broader scientific proposition: that treatment-resistant schizophrenia may stem from dysfunctional neural circuitry rather than dopamine signalling alone.
The limits of dopamine
For more than half a century, schizophrenia pharmacology has centred on dopamine D2 receptor blockade. These drugs reduce psychotic symptoms by suppressing excess dopamine signalling. For many patients, they work. But for a substantial minority, they do not.
After two failed antipsychotics, clozapine remains the standard of care. Yet even clozapine does not consistently eliminate symptoms, and its monitoring requirements and adverse-effect burden limit use. Treatment-resistant schizophrenia is estimated to affect roughly one-third of patients with the disorder.
Increasingly, researchers question whether dopamine dysregulation is the initiating defect in these patients. As Anthony Grace, PhD, a neuroscientist at the University of Pittsburgh, recently told Psychiatric Times: “More recent literature has suggested that the dopamine system is not the site of the deficit. The site of the deficit appears to be in the hippocampus, and hippocampal hyperactivity.” Dr. Grace also pointed to research suggesting that dopamine activity may not be elevated in treatment-resistant patients, potentially explaining reduced response to D2 antagonists.
From receptors to circuits
Evenamide is built around that upstream hypothesis. Rather than blocking dopamine receptors, it selectively modulates voltage-gated sodium channels to dampen pathological neuronal hyperexcitability. According to the company, the drug exhibits no biological activity across more than 130 other central nervous system targets, suggesting a relatively focused mechanism.
Newron says the compound normalises aberrant glutamate release without affecting baseline levels. In preclinical models, combinations of subtherapeutic doses of evenamide and antipsychotics, including clozapine, were associated with benefit, pointing to potential mechanistic synergy.
Researchers argue that this approach could extend beyond psychosis alone. Dr. Grace stated that “by fixing the hippocampus, evenamide has the potential to improve all three major symptom groups, positive, negative, and cognitive, something standard dopamine-blocking drugs cannot do.”
If validated, that broader symptom coverage would mark a departure from traditional antipsychotics, which primarily address hallucinations and delusions. Negative symptoms such as social withdrawal and emotional blunting, along with cognitive impairment, remain closely linked to long-term disability and are among the least effectively treated dimensions of schizophrenia.
Dr. Grace also argues that because evenamide does not block dopamine receptors, it may avoid movement disorders, hyperprolactinaemia and affective blunting commonly associated with D2 antagonists. Early clinical studies, he noted, have shown tolerability comparable to placebo, though those findings will require confirmation in larger trials.
While many next-generation therapies continue to focus predominantly on positive symptoms, attempts to directly target cognition or negative symptoms have repeatedly faltered in late-stage development. Against that backdrop, claims of broader symptom coverage remain ambitious and will ultimately require robust Phase III validation.
Stefan Weber, CEO of Newron Pharmaceuticals, told European Biotechnology Magazine: “Evenamide is a new chemical entity with a unique mechanism of action distinct from all currently marketed antipsychotics. Through novel glutamatergic modulation, evenamide represents a first-in-class approach aimed at addressing the unmet needs of patients with schizophrenia who are poor responders or resistant to existing treatments. Evenamide thus offers hope for the vast majority of patients living with schizophrenia, who currently have limited or no effective treatment options available.”
A field haunted by setbacks, and still expanding
The field’s recent history tempers enthusiasm. Several high-profile programmes targeting novel, non-dopaminergic mechanisms have struggled to translate promising biology into consistent late-stage clinical success. Large pharmaceutical groups have reported disappointing mid- and late-stage results across approaches aimed at muscarinic modulation, glutamatergic pathways, cognitive impairment and TAAR1 activation.
Yet these setbacks have not reversed the scientific trajectory. Academic reviews increasingly frame the next wave as “circuit” medicines, targeting glutamate/GABA microcircuits upstream of dopamine, placing sodium-channel modulators such as evenamide within a broader shift beyond D2-only therapy.
Commercial activity has not slowed either. Industry analyses indicate that more than 55 companies are advancing over 60 schizophrenia therapies across development stages, spanning muscarinic agonists, TAAR1 modulators, serotonin-dopamine agents, long-acting injectables and circuit-based approaches. The breadth of mechanisms underscores both scientific uncertainty and sustained commercial interest in redefining treatment.
Regulatory momentum has also shifted. The US approval of xanomeline–trospium (Cobenfy), described as the first non-dopaminergic antipsychotic in decades, signalled openness to alternative biology and revived investor appetite for mechanistic diversification.
A decisive test
Newron’s ENIGMA-TRS programme comprises two global Phase III studies: a one-year, double-blind trial enrolling at least 600 patients, and a 12-week pivotal study enrolling at least 400. Both evaluate evenamide as an add-on to existing antipsychotics, including clozapine. The final €12mn tranche of the financing is contingent on positive results from those trials, a structure that underscores both investor caution and clinical confidence.
If successful, evenamide would not displace dopamine antagonists. Instead, it could become the first add-on therapy specifically positioned for patients who remain symptomatic despite standard treatment, a potentially meaningful shift in a field long defined by receptor blockade. The decisive test will come with the Phase III data expected in late 2026.


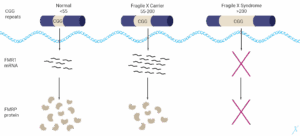 FRAXA Ewsearch Organisation
FRAXA Ewsearch Organisation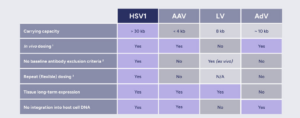 EG 427
EG 427 Nxtera Pharma Ltd
Nxtera Pharma Ltd