Closing the gap in haemophilia therapy
About 25% of the people who suffer from haemophilia A have no therapeutic options, because their immune system forms antibodies against clotting products that can stop bleeding. Researchers and companies in the growing US$15.8bn haemophilia market are feverishly exploring new ways to identify patients at risk and offer them alternative treatments. A series of mergers and acquisitions have changed the playing field for established markets and players.
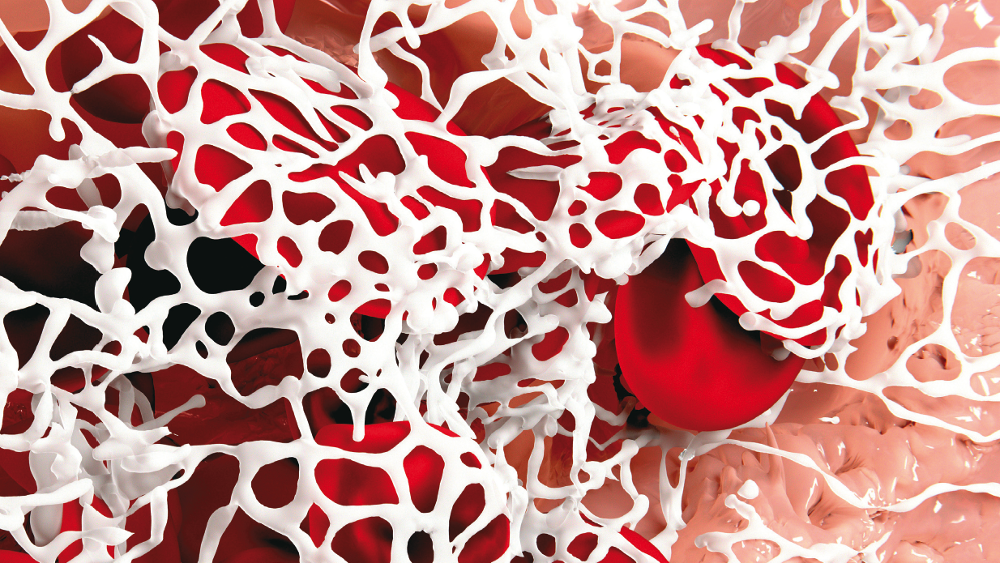
Every time Michael fell when he was a child, his parents had to rush him to the hospital. Between the ages of one and six, we were there pretty much every day, his mother remembers. Her son is one of 320,000 people worldwide with haemophilia A, the more common form of the genetic condition. People living with the hereditary disease either don’t produce enough of a clotting protein called factor VIII, or they lack it completely. Because their blood doesn’t clot properly, it can lead to uncontrolled bleeding. The disease is called mild’ when FVIII levels are 5%-40% of normal levels, moderate’ when between 1%-5%, and severe’ when they’re under 1%. Michael has the severe form. Injections with factor VIII, the current standard of care, can prevent and treat bleeding episodes. Try to do what I can, and not spend too much time thinking about what I can’t do, says Michael, now a young man. For me, that’s a kind of motto in life. Starting in the 1950s, prophylactic factor VIII infusions were derived to treat haemophiliacs with plasma-derived factor VIII products from donors. In the 1990s, complementary treatments with recombinant factor VIII proteins hit the scene.
Prophylactic factor VIII replacement therapy has now cut the average number of bleeds from more than 40 ayear to under two. Today, a child born with severe haemophilia can expect to have a normal lifespan. But besides annual treatment costs of US$150,000-$300,000 per patient, other serious hurdles remain. Prophylactic therapy patients continue to need drugs that will decrease their need for immunosuppressants. The half-life of the active factor VIII protein is also short, and needs to be extended. And most importantly, a significant number of patients simply don’t respond to treatment. Almost one in three people with severe haemophilia A also develops inhibitors – antibodies that identify the recombinant blood clotting factor VIII as foreign, and stop it from working. For the big players in the currently US$15.8bn field – Shire, Biogen/Bioverativ, Novo Nordisk, Pfizer and others – new approaches to solving those problems could have a big impact on revenues. The market is growing. Analysts from Transparency Market Research predict it will surpass US$25bn by 2024.
The huge unmet medical need and associated potential has triggered major acquisitions,with former market leaders under new ownership. Biogen haemophilia spinout Bioverativ, for instance, was taken over by Sanofi for US$11.8bn. In aUS$62bn acquisition, haemophilia amd haematology giant Shire plc agreed in May to a takeover by Takeda. Approaches for circumventing the immunogenicity and inhibitor problem – such as factor VIIIproducts with fully human glycosylationpatterns, gene therapies or bispecific antibodies that mimic the effects of factor VIII with less or no potential for inhibitor formation- have the potential to change the field dramatically.
Predicting inhibitor formation
However, current claims involving reduced immunogenicity and reduced potential for inhibitor formation are still speculative, say haemophila experts like Kenneth Lieuw (J Blood Med, 8;67-73).
Evidence from a 2016 study (NEJM, 374, p. 2054-2064) suggesting that patients who received recombinant factor VIII products had a higher risk of developing anti-factor VIII antibodies than people receiving plasma-derived factor VIII was not confirmed in a 2017 analysis conducted by the European Medicines Agency. The EMA subsequently concluded that the risk of inhibitor development should be evaluated individually for each medicine, regardless of class.
It still isn’t clear though what exactly determines the immunogenicity of factor VIII products – and thus their efficacy. It appears to involve ethnicity (black people are twice as likely to develop problems as white people), genetic mutation (particularly in the F8 gene), and environmental factors.
Also under discussion are the differences in post-translational modification patterns of FVIII. These appear to depend on the cell line used – whether non-mammalian cell lines (e.g., CHO or BHK) or human cell lines (HEK) – and the role played by the factor VIII chaperone (VWF) in both increasing the halflife of FVIII and reducing the endocytosis of FVIII by antigen-presenting cells. Researchrecently showed that second generation products had higher inhibitor rates than third-generation products.
And the experts also say claims that factor VIII products with extended half-lives are also less immunogenic still have to be proven clinically. Investigations into extending the half-life of current recombinant coagulation factors have taken a range of approaches, including reduction of exposure to clearance receptors through PEGylation, rescue of endocytosed proteins from intracellular degradation by crystallizable fragment (Fc) fusion and albumin fusion proteins, and enhanced interactions with VWF.
At the end of March, immunologists at the German regulatory authority Paul Ehrlich Institute reported that bacterial danger signals such as lipopolysaccharide (LPS) in the blood boost T-cell mediated immune responses against factor VIII. The team led by Zoe Waibler said that LPS co-administered with a factor VIII product increased the amount of activated antigen-presenting dendritic cells (DCs) versus factor VIII alone. However, more research has to be carried out to find biomarkers that accurately identify untreated patients
with a high risk for inhibitor formation.
The dawn of a new age in the field – bispecific antibodies and gene therapies
A closely watched drug in the haemophilia A field is Roche’s recently approved, once-weekly bispecific antibody Hemlibra (emicizumab). With one of its two Fab-arms the new medicine approved to treat people with haemophilia A with inhibitors binds to Factor IXa and Factor X, mimicking the role that factor VIII plays in the blood-clotting cascade, particularly the intrinsic activation of platelets.
Results from late-stage pivotal studies show that Hemlibra reduced bleeding rates significantly. Lead investigators stressed that five deaths that occurred in clinical testing were not attributable to the bispecific antibody. In May, however, after 600 patients had been treated with the factor VIII alternative, Roche announced the first patient-terminated Hemlibra therapy after the subject formed antibodies against emicizumab. Circumventing factor VIII administration therefore appears to not necessarily be a long-term solution to the problem of inhibitor formation. Despite that outlook, analysts predict peak sales of US$4bn for Hemlibra – even before Roche applied to extend the label significantly through an FDA-accepted Supplemental Biologics License Application (sBLA) in June. Data from a subgroup of the company’s Haven 3 study suggest that Hemlibra could additionally outperform current plasma-derived or recombinantly produced factor VIII medicines by reducing bleeds more effectively than the current standard strategy for non-inhibitor forming haemophilia A patients. Based on a subgroup analysis of its haemophilia study population of 152 subjects, Roche announced that Hemlibra demonstrated a statistically significant reduction of 68% in treated bleeds after switching from factor VIII products to Hemlibra. That makes it the first medicine to show superior efficacy to prior treatment with factor VIII prophylaxis, the standard of care.
Competitors appear concerned Roche’s antibody could put pressure on their factor VIII products. Even before its board accepted Takeda’s takeover bid, Shire filed an injunction against Roche, claiming the Swiss drugmaker had spread an inaccurate and misleading characterisation of the serious adverse events that occurred in the HAVEN 1 [study] and had also disparaged the safety of Shire’s own bypassing agent FEIBA (factor VIII inhibitor bypassing activity). It contains proenzymes from the prothrombin complex factors, prothrombin, FVII, FIX and FX, but only very small amounts of their activation products, except FVIIa. As real-world benefits of Hemlibra in preventing anti-antibodies have yet to be proven, gene therapies are currently gaining momentum in the public eye, even though all are only in early development stages.
Boost for gene therapies
At the May meeting of the board from the Alliance for Regenerative Medicine, FDA Commissioner Scott Gottlieb announced that the agency plans to accelerate market approval for haemophilia A gene therapies. The FDA wants to approve products based on the levels of factor VIII that patients produce after treatment, as opposed to counting numbers of retrospective bleeds. Within that framework, some US companies
have generated interesting results In a Phase I/II study, BioMarin Pharmaceutical found hints that a dose of
6×1013 vg/kg of its AAV-delivered gene therapy valoctocogene roxaparvovec (BMN270) raised factor VIII levels to 59% after 24 months of treatment. Mean factor VIII usage was reduced by 96% through a single injection of the gene therapy. Enrolment for the ongoing pivotal GENEr8-1 Phase III trial on 130 patients will be complete next year.
Pfizer and Sangamo Biosciences, which raised US$200m in April, are also in Phase I/II testing of the AAV-delivered factor VIII gene therapy SB-525. And Shire/Takeda have an AAV8-based gene therapy in Phase I testing that was renamed from BAX 888 to SHP654, following the 2016 Baxalta takeover. Last but not least, Dutch UniQure N.V. also has a gene therapy in the pipeline. Gene therapies have potential drawbacks, among them the risk of developing antibodies to the viral vectors used to deliver the genetic material to cells. According to Bioverativ, there’s still a long way to go in establishing safety, efficacy and durability in the field, so recombinant factor VIII products will certainly play a leading role for many years to come. After all, people with haemophilia A like Michael tend to be highly averse to risk.
First published in European Biotechnology, Summer 2018 edition



 adobe.stock.com - ipopba
adobe.stock.com - ipopba BioDlink
BioDlink