Researchers stop brain cell death in Alzheimer’s mice
A Belgian-British research team has identified the human protein underlying necroptosis of human brain cells in Alzheimer's mice and stopped cell death.
The research team led by Prof. Bart De Strooper (VIB-KU Leuven/UK Dementia Research Institute), and Dr Sriram Balusu (VIB-KU Leuven) has finally discovered how neurons die in Alzheimer’s disease. When human neurons implanted into the brain of Alzheimer mice were exposed to amyloid plaques and Tau tangles – the hallmark misfolded proteins implicated in Alzheimer’s, human neurons – in contrast to mouse neurons – initiated a programmed cell death form dubbed necroptosis. More importantly, the researchers were able to prevent necroptosis opening new pathways for potential treatments.
Whether the discovery is good news for the six to seven million patients who are diagnosed with Alzheimer’s disease (AD) has to be proven in clinical trials yet. However, the discovery of a completely new biological mechanism for AD, for the first time provides an explanation on how accumulation of protein plaques and tangles are linked to cell death in human brains.
Our study sheds light on the previously murky waters of Alzheimer’s disease, revealing a potential key player in neuronal loss – a RNA gene called MEG3, and the process of necroptosis,” said De Strooper. “These findings are an important step forward in furthering our understanding of the basic mechanisms underlying this complex and often misunderstood disease.
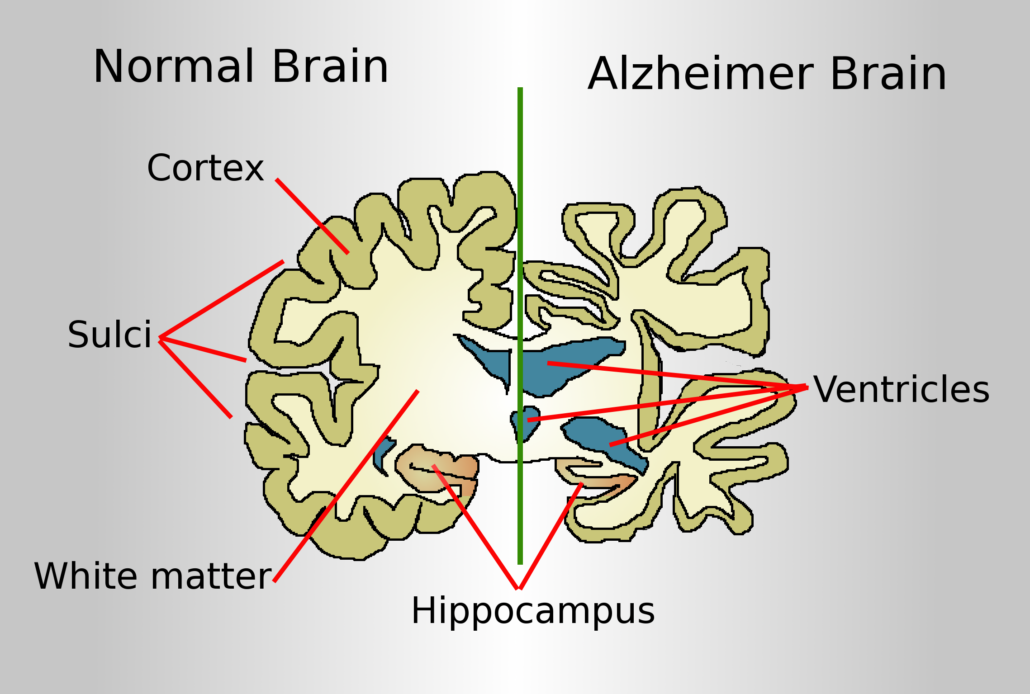
One of the key challenges in understanding Alzheimer’s disease has been connecting its defining hallmarks – amyloid plaques, tau tangles, and death of neurons – to each other. Most mouse models used in research couldn’t naturally replicate the link between AD its defining hallmarks – amyloid plaques, tau tangles, and death of neurons – to each other, leaving scientists with unanswered questions about how they relate to disease progression.
To bridge this gap, we created a new model, says Balusu, postdoctoral researcher at the De Strooper lab and first author of the paper. We implanted both healthy human and mouse neurons into the brains of AD mouse models. The human cells degenerated much like their counterparts in the human brain, allowing us to study them during brain ageing and shine a new light on the processes underlying AD.
Remarkably, only the human neurons, and not their rodent counterparts, displayed AD features seen in the brains of patients, including tau tangles, and significant neuronal cell loss. Specifically, human neurons xenografted in mouse brain exposed to amyloid pathology developed sarkosyl-insoluble tau filaments, positive Gallyas silver staining, release phosphorylated tau (P-tau181) into the blood, and display considerable neuronal cell loss, providing a model for the induction of full Tau pathology by simple exposure to amyloid pathology in AD. This suggested that there may be human-specific factors at play in AD that standard mouse models can’t replicate. Understanding why mouse neurons are more resilient to amyloid pathology will not only help model the disease better but might also stimulate research into pathways that protect against neurodegeneration.
Using their new model, the team probed deeper, seeking answers on how neurons die in AD. The study revealed a critical breakthrough: a pathway known as necroptosis, a form of programmed cell death, was activated in the model, leading to death of neurons. But the discovery went even further. The researchers saw that levels of a long non-coding RNA known as MEG3 was strongly increased in human neurons, as seen in AD patients. Strikingly, just the presence of MEG3 alone was enough to trigger the pathway of necroptosis in human neurons in the lab setting. The study also found that by reducing MEG3 and preventing necroptosis by orally administered small molecule receptor-interacting protein (RIP) kinase -1 and -3 inhibitors in this novel AD model, researchers could in turn prevent the death of cells. More research is needed to understand how exactly MEG3 triggers necroptosis, but this discovery represents a crucial advancement in understanding how Alzheimer’s leads to the loss of neurons in the brain.
Necroptosis is already an active area of drug development in cancer and ALS, says De Strooper. While there’s much more to explore, our findings open up promising avenues for potential therapies targeting AD, alongside traditional approaches aimed at amyloid and tau.




 Tetraneuron SL - Álvaro García
Tetraneuron SL - Álvaro García