Researchers overcome chemotherapy resistance in AML
German researchers have found a biomarker that reliably predicts outcomes of blood cancer treatment with the chemotherapeutic cytarabine. Targeting the biomarker restored cytarabine sensitivity.
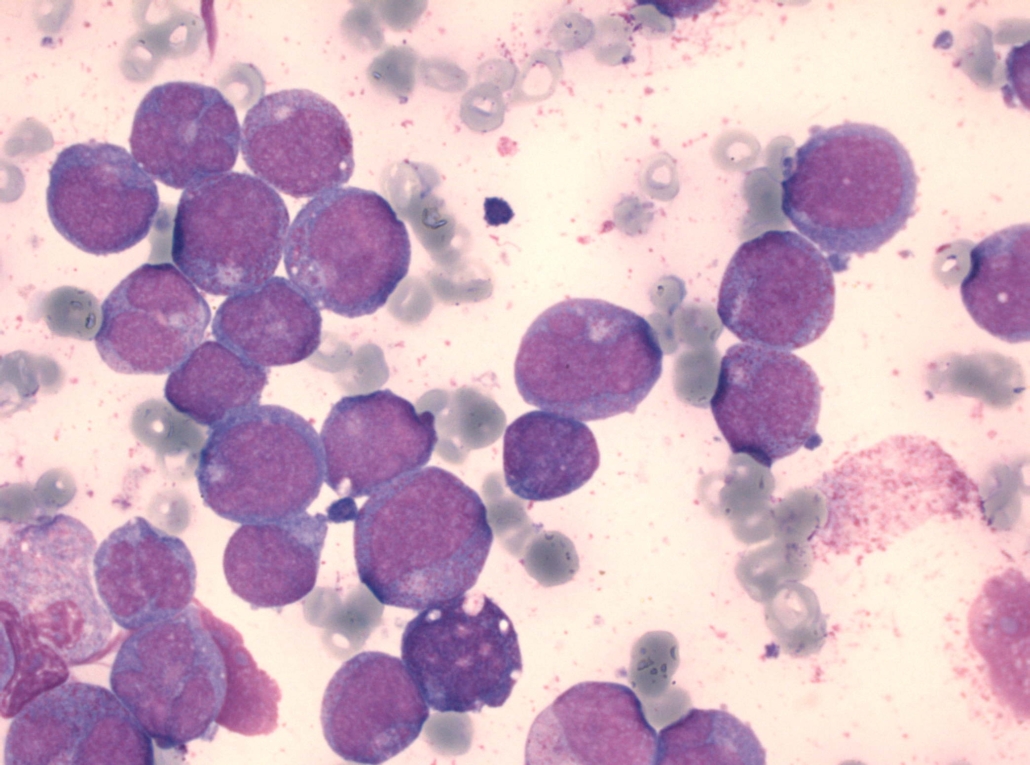
Outcomes in patients with the blood cancer AML (acute myelogenous leukaemia) range from a 70% five-year overall survival (OS) rate among children to a less than 20% two-year OS rate among adults. Lack of response to the DNA synthesis blocker cytarabine (ara-C) is the main cause for treatment failure and relapse. A team headed by Jindrich Cinatl (Goethe-University Frankfurt) now identified the cause for the bad response of AML patients to the nucleotid analogue ara-C, which causes DNA damage through perturbation of DNA synthesis.
Both the cytotoxicity of ara-C, which is part of standard chemotherapy of AML, in vitro and in patients correlate with the ability of AML blasts to accumulate the active metabolite ara-C triphosphate (ara-CTP). Cinatl’s team identified an enzyme that detoxifies intracellular ara-CTP pools by ara-CTPase activity. According to the researchers, the enzyme code-named SAMHD1 could serve both as a biomarker for responsiveness to ara-C therapy but also as a drug target.
Three weeks after the identification of SAMHD1 stratification biomarker by Cinatl, Thomas Helleday (Karolinska Institute, Stockholm) and Torsten Schaller (University Heidelberg) reported that blocking the SAMHD1 gene by CRISPR/Cas9-mediated gene disruption resensitised cancer cells to ara-C treatment. Furthermore, treatment with the Vpx protein of the simian immunodeficiency virus (SIV) dramatically increased sensitivity of primary patient-derived AML blasts to ara-C-induced cytotoxicity. In pediatric and adult AML patient cohorts receiving ara-C treatment, SAMHD1 presence proved to be a risk factor. The research team concluded that SAMHD1 expression levels dictate patient sensitivity to ara-C, providing proof-of-principle that the targeting of SAMHD1 by Vpx could be an attractive therapeutic strategy for potentiating ara-C efficacy in hematological malignancies.



 adobe.stock.com - ipopba
adobe.stock.com - ipopba BioDlink
BioDlink