Blood test predincting Alzheimer’s paves way to earlier therapy
A newly developed blood test indicates Alzheimer's disease on average eight years before the clinical diagnosis.
The results, obtained in a long-term population-based cohort study could pave the way of earlier treatment of risk patients with existing therapies before neurodegeneration has led to irreversible brain damage, the scientists from the University Bochum, the German Cancer Research Center (DKFZ) and the Saarland Cancer Registry suggest
Though there is currently no cure for Alzheimer’s disease, the researchers believe that therapeutic progress has been hampered by the fact that the disease can only be diagnosed when it is too late for an effective intervention. Alzheimer’s disease is assumed to begin 15 to 20 years before patients show typical symptoms like memory loss.
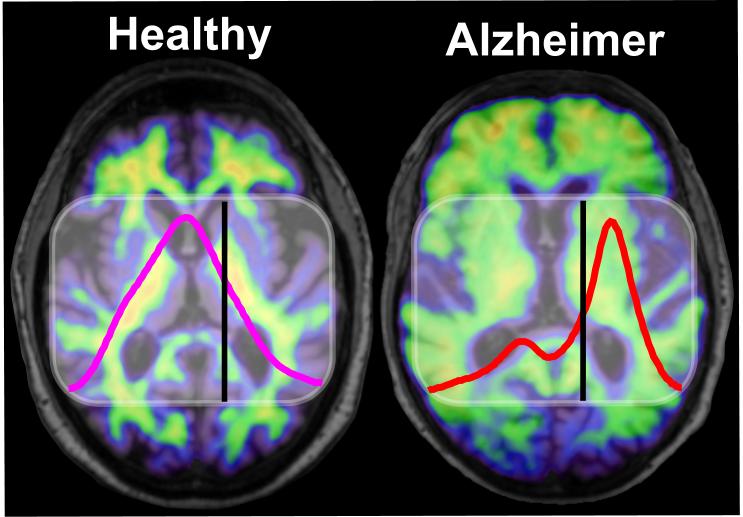
The scientists headed by biophycist Klaus Gerwert used a method dubbed immuno-infrared sensor to measure distribution of pathological and healthy structures of amyloid-? in the blood of people participating in a long-term cohort study over 15 years. The pathological amyloid-? structure, which initiates the formation of toxic plaques in the brain, is rich in a sticky, sheet-like folding pattern that makes it prone to aggregation, while the healthy structure is not. The two structures absorb infrared light at a different frequency (see photo), allowing the blood test to determine the ratio of healthy to pathological amyloid-? in the sample.
The assay was able to detect signs of the disease on average 7.9 years before diagnosis in individuals without clinical symptoms. It correctly identified those with the disease in almost 70% of the cases, while about 9% of true negative subjects would wrongly be detected as positive.
Currently available diagnostic tools for Alzheimer’s disease either involve expensive positron emission tomography (PET) brain scans, or analyze samples of cerebrospinal fluid that are extracted via lumbar puncture. The researchers suggest that their blood test serves as a cheap and simple option to pre-select individuals from the general population for further testing by these more invasive and costly methods to exclude the falsely positive subjects.


 Unsplash+
Unsplash+