AML: Sorafenib boosts graft-versus-leukemia activity
Co-administration of an allogenic blood stem cell transplant and sorafenib cured AML patients refractive to chemotherapy and stem cell transplants alone, oncologists report in Nature Medicine.
"Originally, sorafenib was only given to patients to slow the progression of the disease. We then found that the cancer disappears in patients who had previously received a transplant of healthy immune cells. That surprised us extremely," says study leader Prof. Dr. med. Robert Zeiser, Senior Physician and Head of the Department of Tumour Immunology at University Medical Center Freiburg.
Zeisser’s team showed that sorafenib stimulates the production of the messenger interleukin-15. This leverages the camouflage mechanisms of cancer cells and makes them visible to the immune system (Nature Medicine, doi: 10.1038/nm.4484). Actually, co-administration of an allogenic hematopoetic stem cell transplant (allo-HCT) and sorafenib cured relapsed patients with acute myeloid leukemia (AML) who carry an internal tandem duplication in the FLT3 gene (Fms-related tyrosine kinase 3). Normally, this patient group has a fatal outcome with a 1-year survival rate below 20%. According to Zeiser in many other cases the cancer was strongly suppressed. Relapse occurs in 60% of patients with AML, the most common form of blood cancer. In every eighth AML patient, the cancer can not be repressed in the long term, neither with chemotherapy nor with stem cell transplantation.
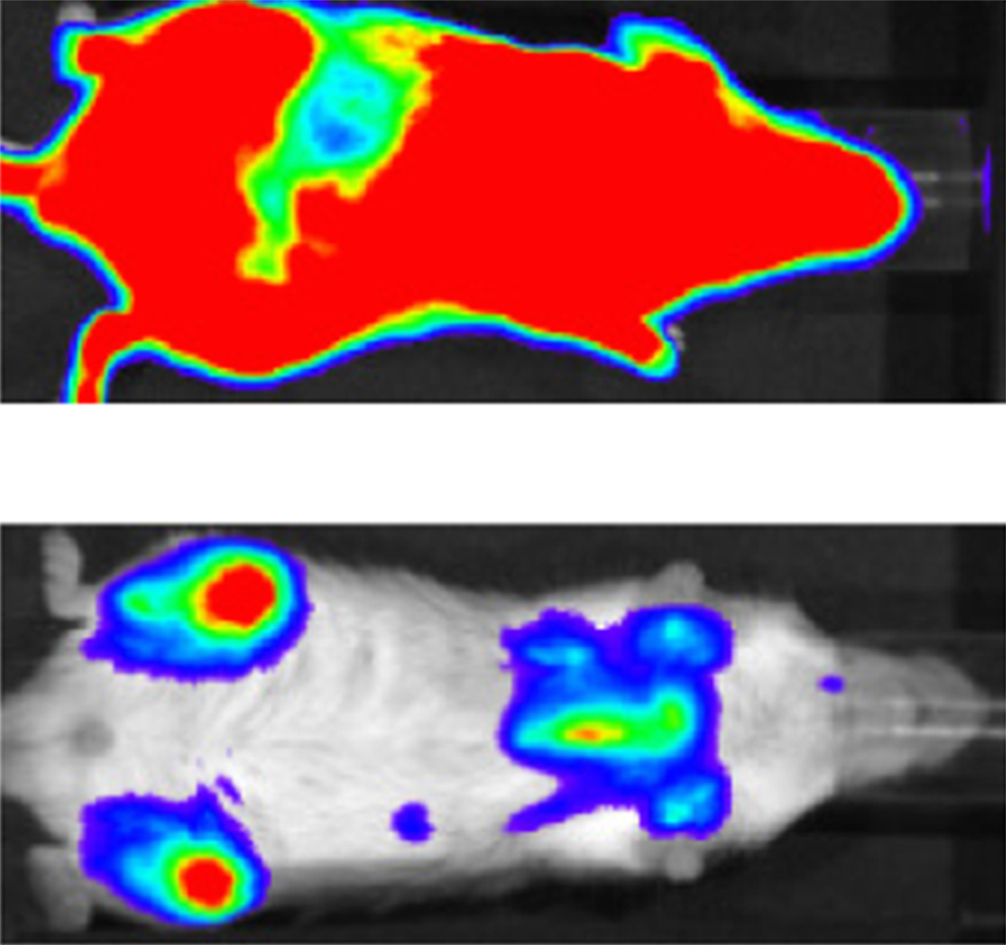
In lab studies, they found out that Bayer’s multi-tyrosine kinase blocker sorafenib worked by increasing IL-15 production in FLT3-ITD+ leukemia cells. This synergized with the allogeneic CD8+ T cell response, leading to long-term survival in six mouse models of FLT3-ITD+ AML. Mechanistically, sorafenib reduced expression of the transcription factor ATF4, thereby blocking negative regulation of interferon regulatory factor 7 (IRF7) activation, which enhanced IL-15 transcription. Both IRF7 knockdown and ATF4 overexpression in leukemia cells antagonized sorafenib-induced IL-15 production in vitro. In animal and human cells increased IL-15 expression coincided with reduced PD-1 levels.
Lab results were confirmed by a large-scale data analysis from more than 409 patients from 39 study centers worldwide. Patients were all treated with various medications due to an AML leukemia relapse. "The combination of sorafenib and T-cell transmission clearly led to the best chance of survival," says Zeiser. Furthermore, human FLT3-ITD+ AML cells obtained from sorafenib responders following sorafenib therapy showed increased levels of IL-15, phosphorylated IRF7, and a transcriptionally active IRF7 chromatin state. The mitochondrial spare respiratory capacity and glycolytic capacity of CD8+ T cells increased upon sorafenib treatment in sorafenib responders but not in nonresponders.
Sorafenib has been granted market authorisation for the treatment of liver, kidney and thyroid cancer. "Because sorafenib is already approved, those affected can be treated immediately," expects Zeiser.



 Unsplash+
Unsplash+