
Hope for more selective cancer antibodies
Monoclonal antibodies still dominate the US$417bn biologics market. After decades of development, however, improved antibodies and protein formats with better target selectivity and safety profiles are now hitting markets and pipelines. A range of bispecific antibodies and antibody-drug conjugates – along with CAR-Ts, TCR-RTs and NK cell-based immunoreceptor constructs – were in focus at the PEGS Europe Summit.
Since the first antibody drug (muromonab-CD3) was approved back in 1986, monoclonal antibodies (mAbs) have emerged as the dominant class in the global US$417bn market for biologics. At the end of 2023, sales stood at more than US$230bn. However, as tumours – in addition to autoimmune diseases still one the most important application fields of mAbs – are moving targets, newly engineered antibody and engineered protein formats that unite complementary cell-killing mechanisms in a single molecule have been developed, approved and are increasingly leaving clinical pipelines for the market. They include refined bispecific antibodies, antibody drug conjugates (ADCs) and targeted radiopharmaceuticals, as well as immune-receptor-based cell therapies such as CAR-T and TCR-T cell therapies.
Every year at the PEGS Europe Summit, the CSOs of bio/pharma companies provide a detailed overview of newly developed therapeutic modalities, and thus an outlook for the future. This year in Barcelona, the 16th summit helped clarify why the approval of bispecific antibody formats has increased dramatically (13 out of 18 approvals in the past three years) and why improved ADCs, CAR-Ts, TCR-Ts and new modalities are entering the market. The freshly engineered formats promise to reduce current problems of bispecific antibody and T-cell therapies such as cytokine release syndrome (CRS), neurotoxicity, and on-target/off-tumour toxicity. In addition, targeting two targets simultaneously increases selectivity, and allows drug developers to combine complementary cancer-killing mechanisms that could reduce resistance to cancer therapies and improve efficacy.
“Based on recent therapeutic progress, ADCs and bispecific antibodies (bsAbs) represent the fastest-growing class of therapeutic antibodies in development and have been a major driver of dealmaking in the biopharmaceutical industry in the past years,” emphasised Dr Christian Klein at the PEGS summit, which took place from 5-7 November. The patent champion (240!) in protein engineering, who moved to early-stage investor Curie.Bio in the summer after 22 years at Roche pRED started with a brief summary of the 14 bispecifics (and 17 – still monospecific – ADCs on the market) approved until December 2023. But he quickly turned to what’s new, interesting and probably a business case. And there is a lot of ground to cover, as around 50% of bispecific antibodies are already in late phase testing (Phase II or III).
New age for bispecifics
According to Klein, T-cell engagers (TCEs), together with cancer immunotherapies, now account for almost 80% of the bispecific antibodies clinically developed to fight cancer. They are also increasingly used in indications beyond haematological cancers, namely solid tumours and autoimmune diseases (TCEs and dual-ligand blockers). Dual-ligand inhibitors such as faricimab (VEGFxAng2) from Roche, which was approved by the FDA in 2022 for the treatment of wet age-related macular degeneration (AMD), have already found their way into ophthalmology. And Sweden’s BioArctic AB is working on an advanced version of Roche pRED’s transferrin receptor-mediated brain shuttle technology, which was presented for the first time at the PEGS Europe Summit. According to data revealed in Barcelona, the brain transporter platform, which was licensed to Esai last year, was able to increase brain exposure to an anti-amyloid beta antibody by 70-fold. Bispecific antibodies in the obesity field have also already been the subject of licencing agreements, such as the as yet unnamed dual activin type IIA and IIB receptor modulator from Swiss SixPeaks Bio AG, for which AstraZeneca has an option since May.
Approvals in 2024
A total of three “classic” TCEs have been given the green light by the regulatory authorities this year, including one for solid tumours. In May, Amgen’s DLLxC3-BiTE format tarlatamab-dlle got FDA approval as a second-line treatment for extensive stage small cell lung cancer (ES-SCLC). In August, Regeneron’s previously FDA-rejected, hinge-stabilised Fc-binding-reduced CD20 x CD3 bispecific IgGπ antibody odronextamab received EU approval as a third-line therapy for patients with follicular lymphoma and diffuse large B-cell lymphoma. Both share the CD3-related (CRS) toxicity of first-generation products. The very first bispecific T cell engager (EpCAM xCD3) Removab (catamaxumab, Trion Pharma) against malignant ascites (approved 2009, withdrawn 2014) is set to be reapproved in the EU and marketed by Lindis Biotech/Pharmanovia later this year. There were also two approvals for candidates with an alternative design:
At the end of November, Zymeworks Inc’s/Jazz Pharmaceuticals Inc’s biparatopic HER2 signalling blocker zanidatamab-hrii got the FDA stamp. Binding of zanidatamab with two different extracellular epitopes on HER2 (D2 + D4), previously targeted separately by Roche’s blockbuster HER2 antibodies Herceptin and Perjeta, results in internalisation leading to a reduction of the receptor on the tumour cell surface. It unites three tumour cellkilling mechanisms in one antibody: CDC (complement-dependent cytotoxicity), ADCC (antibody-dependent cellular cytotoxicity) and ADCP (antibodydependent cellular phagocytosis). According to Klein, combining MoAs that are not accessible to monoclonal antibodies exactly is what makes some of the novel bispecific constructs so interesting.
Another new approach, pioneered by Chinese biotech Akeso Biopharma Co. Ltd, is combining different immune checkpoint inhibitors in a bispecific antibody. Back in 2022, Akeso Bio received NMPA approval for the very first-(PD1 x CTLA4) drug in this new class of cancer immune therapies. Interest in a bispecific combination that unites checkpoint inhibition with angiogenesis through PD-(L)1xVEGF bispecific antibodies blew up after Akeso Bio and Summit Therapeutics celebrated a first-time victory of ivonescimab (SMT112) over MSD’s US$15bn per year blockbuster pembrolizumab in a head-to-head Phase III trial. That was followed by approval of the drug in China as a first-line NSCLC treatment. The results – objective response rates were 50% with ivonescimab versus 38.5% with pembrolizumab, disease control rates were 89.9% and 70.5%, respectively – is still sending shockwaves through the immuno-oncology industry.
In the field of haematological and solid cancers, what is still the dominant application field (73% solid tumours) of the currently more than 50 different formats of bispecific antibodies, dual receptor tyrosine kinase blockers and biparatopic constructs such as zanidatamab are only one approach that will increasingly see clinical uptake. The overall goal of all developers of new T-cell engaging approaches, bispecific ADCs etc. is to increase tumour selectivity, eliminate tumour escape and reduce dose-limiting systemic toxicities. Also to hinder the T-cell exhaustion that often leads to relapse or non-responsiveness to redirected T-cell therapies. Several strategies discussed at PEGS Europe by start-ups and biopharma companies address this problem.
Early-stage approaches
Yemi Onakunle, CEO of Mabswitch Inc (Los Angeles), presented a completely new technology in Barcelona that allows switching the T-cell binding affinity. According to him, this is instrumental to ameliorate TCE and CAR-T cell-therapy intrinsic toxicities caused by T-cell hyperactivation and chronic antigen stimulation. What he called “remote control” of an antibody’s affinity is achieved by inserting a universal calmodulin-derived allosteric modulator domain between the two protein domains (VH/VL), which affects the molecular geometry of the antigen binding site of the antibody. The modulator – or “switch” – can be modulated itself electrostatically by a range of small molecules that can be added or removed. Onakunle showed data from Off- and On-switches for TCEs, CAR-Ts, ADCs or protein purification applications that altered the affinity of antibodies by two orders of magnitude. The universal allosteric affinity-switch worked independently of the paratope. The approach of the three-year old start-up, co-founded by Phage display co-inventor Stefan Dübel, enables both increased and decreased affinity in antibodies, offering a tunable strategy to enhance CAR T cell or T-cell engager safety and efficacy in patients.
Other approaches aim to circumvent T-cell-born safety issues by using alternative effector cells, namely NK or so-called MAIT cells. Simon Plyte, CSO of Biomunex Pharmaceuticals SA (Paris), said using an abundant tissue and tumour resident subset of cytotoxic non-conventional T cells that make up 20% of the T cell population could significantly widen the therapeutic index of T cell therapies. While the proprietary, bispecific BiXAb antibody-mediated redirection of these MAIT cells (Mucosal Associated Invariant T cells) to TAAs lead to the elimination of cancer cells with a potency identical to that of classical CD3e T-cell engagers, MAIT engagers triggered neither cytokine release syndrome nor regulatory T-cell activation, because they are activated through binding to the iTCR. According to data shown by Plyte, tumour-resident MAIT cells are able to eliminate autologous tumour cells in a MAIT-engager mediated manner, and can infiltrate and kill tumour cells in patient-derived 3D models of cancer.
Another approach, chosen by French Innate Pharma SA, which also has fourth-generation ADCs in its portfolio, is to circumvent the T-cell-specific problems by using NK cells that neither induce CRS nor activate CD25+ regulatory T cells. The company’s tetraspecific B and NK cell engager IPH6501 exhibited higher anti-tumour efficacy and lower systemic toxicity than CD20-targeting TCEs. The candidate currently undergoing Phase I/II trials, engaged NK cell-activating receptors (NKp46 and CD16), the CD20 TAA on B cell blasts and includes an IL-2 variant designed to avoid binding to CD25, limiting Treg activation and potential IL-2 related side effects (see p. 70).
Local activation
In addition to these innate cell engagers, approaches in which probodies are first activated in the tumour were also discussed at PEGS Europe. Here, the binding sites are initially masked sterically or by attaching protective groups, which are cleaved off by TME specific proteases. Or they are engineered to be active only at acidic pH or high ATP concentrations. An alternative approach for dual tumour targeting at an early stage is based on the tumour-specific composition of a functional CD3e antibody fragment consisting of two bispecific antibodies with split CD3e binding moieties. These units must be designed to be inactive and circulate as separate units so that they are activated only after binding of the tumour antigen and subsequent in situ assembly. However, it is tricky to produce the monomers because they tend to aggregate in solution.
At PEGS Europe, Thomas Spreter von Kreudenstein, Senior Director Protein Engineering and Multispecific Antibody Technologies at Zymeworks, presented a new conditional masking approach for Zymeworks’ cIL-12 cytokine fusion protein ZW270. Though IL-12 drugs have already shown the ability to turn ‘cold’ tumours ‘hot’, they also delivered poor responses – most likely due to toxicity and thus a low therapeutic index. After optimisation, an attenuated, masked IL-12 Fc (ZW270) showed anti-tumour efficacy in a humanised syngeneic mouse model in a dose range from 0.5 mg/kg-32 mg/kg, while reference mice with unmasked wild-type IL-12 showed a maximal tolerated dose of less than 0.05 mg/kg. Testing is ongoing.
ADCs and radio-DARPiNs
While the 13 approved antibody-drug conjugates (ADCs) enable the selective delivery of highly cytotoxic payloads linked to a tumour-targeting antibody with 50%-60% objective response rate on average, challenges such as drug resistance, tumour heterogeneity and treatment-related adverse effects continue to hamper the medical success of this drug class, which saw its first approval in 2000 with Pfizer’s second-line CD33-positive AML therapy Gemtuzumab ozogamicin.
Different engineered ADC formats and – above all – new payloads were discussed at the PEGS Europe Summit, with the goal of widening the still too-narrow therapeutic index of the rapidly growing clinical pipeline (300 INDs this year, mostly in China, which holds 42% of it). New formats discussed included bispecific ADCs, conditionally active ADCs, immune-stimulating ADCs, protein-degrader ADCs and dual-payload ADCs. Premature payload release, poor tumour penetration, variable drug-to-antibody ratios and aggregation were the topics discussed most.
Joost Uitdehaag, Head of Biology at Crossfire Oncology BV, underlined the need for new non-chemical payloads, because these most common payloads limit the application of ADCs due to their high systemic toxicity. He highlighted kinase degraders targeting cancer-driving proteins, because the 80 approved kinase blockers would have better selectivity and are less toxic than anti-mitotics, tubulins and topoisomerase I blockers. He reported on a Phase I-ready novel cell cycle kinase degrader payload called CFON 18801, which was screened from 300 candidates with kinase and cell-based HIBIT assays, and its application as part of a Degrader-Antibody-Conjugate (DAC) to target metastatic castration-resistant prostate cancer (mCRPC). In vitro, CFON 18801 showed a DC50 in the single-digit nM range, and completely arrested the cell cycle in S-Phase by full target degradation within 254 hours, inducing strong immunogenic cell death. CFONs allow a drug-to-antibody ratio from 2-8. Conjugation of CFON 18801 to an prostate cancer-specific antibody showed picomolar cytotoxic activity outperforming a doxorubicin-based conjugate. Its in vivo efficacy is currently being assessed.
Justyna Mysliwy, Senior Director of Research at Iksuda Therapeutics Ltd in Newcastle’s Biosphere Life Science Ecosystem, presented the company’s intratumourally activated ADCs. Not long ago, the first HER2-positive breast, lung and gastric cancer patient was enrolled in a doseescalation study of Iksuda’s lead candidate IKS104. The firm’s Chinese partner Fosun is already testing the probody ADC in Phase II/III trials, which is cleaved at low pH by the cancer lysosome-selective enzyme beta-glucuronidase, thus avoiding the risk of on-target, off-site toxicity. The probody carries two PDB payloads per molecule.
Conjugation impact
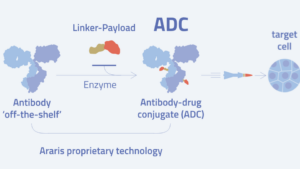
A novel conjugation approach was presented by David Spycher, CSO of Zürich-based Araris Biotech AG. Using microbial transglutaminase, Araris was able to link short, positively charged lysine-containing peptides to HER2-targeting antibodies at their residue glutamine 295 (Q295) without the need for any protein engineering and at a stochiometric drug-to-antibody ratio of 2 or 4. When a-amanitin was used as a toxic payload, complete and long-lasting tumour remission was achieved together with highly reduced toxicity at all dose levels tested. Quantitative biodistribution studies performed with 111In-radiolabeled conjugates showed high tumour uptake and low accumulation of radioactivity in non-targeted tissues.
After raising €54m in Series A financing, Belgian ADC maker ATB Therapeutics BV now claims its technology has solved bioconjugation-related problems. The ATBioFarm platform allows for one-step production of ADCs in tobacco plants. They consist of a targeting antibody, a cleavable but stable peptidic linker and a cell-killing enzymatic payload, and are made by just transferring the encoding DNA sequence into a tobacco-compatible vector that is expressed within the plant cells. According to the technology’s inventor COO Max Houry, the ADC-like fusion proteins circumvent common problems of bacterial and mammalian expression systems that occur in the process of attaching toxic payloads in a defined stochiometry to the targeting antibody. Additionally, in contrast to typical payloads, ATbodies use enzymatic cell-killing mechanisms that are complementary to the mode of action of chemotherapeutics
Andreas Bosshard from Molecular Partners AG explained ways of reducing the renal toxicity of radio-Darpin conjugates derived from ankyrin-repeat proteins. To minimise accumulation of radioisotopes in the renal glomerulus, Darpins were produced in which positive surface charges were partly or fully exchanged with negative ones. Although radio-Darpins with fully exchanged charges were significantly less toxic, they were also less effective in reaching the tumour.
Bispecific ADCs also show increased tumour selectivity. Last December, Bristol Myers Squibb licenced global, ex-China rights for the Phase III first-in-class bispecific (EGFRxHER3) ADC izalontamab brengitecan (BL-B01D1) from Chinese SystImmune Co. Ltd for US$800m up-front plus US$500m near-term payments in a US$8.4bn biobucks deal. As the toxic camptothecin payload (DAR 7.5-8) still belongs to the classical payload trio – supertoxic anti-mitotics, DNA alkylating agents and dominating topoisomerase 1 inhibitors (53%) – the recommended dose in humans is still low (2.5mg/kg, preclinically 10 mg/kg) and miles away from what is regarded as optimal for good biodistribution (6-10 mg/kg, see interview p. 40). However, the reported objective response rate was 60% in Phase I/II, with neutropenia as the most reported adverse effect (ADE).
A new approach?
A discovery by scientists at the University of Pittsburgh and the UPMC Hillman Cancer Center is kindling hopes of ending the stealth strategies of solid tumours that put immune cell therapeutics to sleep in the TME once and for all. The team discovered that lactic acid pumped out of the tumour appears to contribute significantly to so-called T-cell exhaustion. At the same time, they discovered that this lactate sensitivity disappears when they blocked the T-cell lactate transporter MCT11 with antibodies (Nature Immunology, doi: 10.1038/s41590-024-01999-3). The antibody, which significantly improved the control of tumour growth in mice, is now to be tested clinically. “Blocking access to inhibitory metabolites is a completely new approach to how we can reactivate the immune system,” said lead author Greg Delgoffe, Director of the Tumour Microenvironment Center at UPMC Hillman. “If we get rid of MCT11, there is no difference in the expression of co-inhibitory receptors on T cells,” Delgoffe added. “MCT11 is an attractive therapeutic target because it is almost exclusively expressed by exhausted T cells that concentrate in tumours. This makes it a potentially more selective and targeted treatment option compared to other immunotherapies, such as PD1 checkpoint blockers.” Bispecific (PD1 x MCT11) Innate engagers could therefore be a future option in the ongoing fight against cancer.
t.gabrielczyk@biocom.de


 Araris Biotech AG
Araris Biotech AG Lonza Group
Lonza Group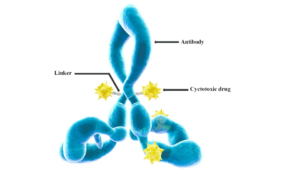 International Journal of Molecular Sciences, doi: 10.3390/ijms17040561 JO - s
International Journal of Molecular Sciences, doi: 10.3390/ijms17040561 JO - s