GMP and new processes: be prepared for hassle
Poor aseptic practices can rapidly ruin market supply of products outsourced for production. This year, Celltrion came under fire from FDA inspectors. At the end of January, the producer received a warning letter affecting the production of Inflectra biosimilar infliximab-dyyb (CT- P13) co-marketed with Pfizer. In mid-February, the FDA added a warning concerning rituximab and trastuzumab biosimilars produced for Teva, as well as for its fast-track migraine mAb fremanezumab.
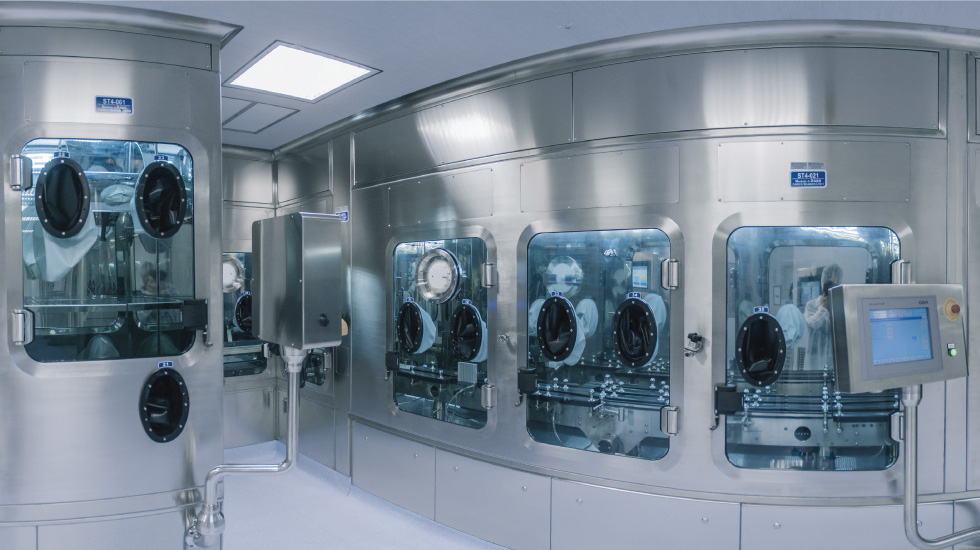
The warning letter resulted from inspections of the South Korean biosimilar specialist’s current 140,000-litre production plant in Incheon conducted last summer. According to the FDA, it followed about 140 complaints concerning contaminations in vials due to insufficient sterile filling procedures affecting products marketed in the US. The contamination problem could affect US and EU market approval for Celltrion’s trastuzumab biosimilar CT-P6, which had its BLA accepted by the FDA and received recommendation by the CHMP, bothlast year, and FDA approval of the EU-authorised rituximab Truxima. According to Teva, the warning letter could also ruin the planned marketing debut of its anti-CGRP mAb fremanezumab that prevents migraine attacks. In January, the FDA issued a warning letter to Celltrion and its global co-marketing partner Pfizer Inc. concerning infliximab-dyyb, a biosimilar of the autoimmune blockbuster Remicade (infliximab) from Johnson & Johnson, the first biosimilar mAb approved by the agency in 2016. For Celltrion, which is playing down any concerns related to its expanding biomanufacturing plant in Incheon, the warning letters could have a huge impact on its business. Celltrion, which will ramp up its capacity to 310,000 litres by 2019, wanted to outperform European CDMO rivals Boehringer Ingelheim (300,000 litres) and Lonza (280,000 litres). Samsung Biologics Co., another Korean producer of biologic drugs, has a plan to increase its annual production capacity to 360,000 litres by 2018.
he GMP issues at Celltrion come at a time in which healthcare systems have begun to lobby for adoption of the 15-30% cheaper versions of biologics that have lost patent protection. Australia, following the European practice, no longer labels the INN of biosimilars with a unique numerical identifier to differentiate them from the originals. Though the FDA includes the unique INN identifier for biosimilars, the US government wants to boost biosimilar uptake. At the beginning of February, FDA Commissioner Scott Gottlieb announced the agency will facilitate claims of interchangeability in a forthcoming Biosimilars Innovation Plan, which could promote biosimilar uptake.
Find the right expert
While most GMP problems are currently limited to Indian, Chinese, and other CDMOs from Asia, some have also hit Western companies, such as Pfizer subsidiary Meridian Medical Technologies Inc., whose QC did not meet cGMP requirements, causing the FDA to to reject AstraZeneca’s market approval application for ZS-9, an ion trap to treat hyperkalemia.
The cases document what really counts for biopharmaceutical companies: quality and price, but quality first. In Europe, smaller specialised biomanufacturers have found a niche in the innovative biotech SME space, providing special expertise suited to the needs of their customers. CDMOs, such as Celonic, no longer want to remain just the lot-makers for clinical trials but have begun to expand into the high-quality commercial production of personalised meds, orphan drugs, etc. Most recently, Celonic took over the manufacturing business from protein glycosylation specialist Glycotope and is also expanding its production capabilities in Basel.
Another tactic to differentiate within the consolidating, but growing, outsourcing market – which had sales of US$5.48bn, according to Visiongain analysts – is to provide novel technologies in selected drug discovery areas for customers.
In February, Teva partnered to get access to ProBioGen’s Human Artificial Lymph Node Technology, a 3D-micro-organoid model for predicting the effects of Teva’s biopharmaceutical drug candidates on the human immune system in vitro. ProBioGen’s CSO, Dr. Volker Sandig, said, We have demonstrated effects that were impossible to see in conventional models, bridging the existing gap between animal models and first-in-man applications. The technology is based on a patented, miniaturised, and perfused bioreactor for long-term cultivation of immune cells. Human blood-derived dendritic cells, lymphocytes, and mesenchymal stem cell-derived stromal cells are inoculated into the bioreactor’s 3D hydrogel matrix, which is perfused with cell culture medium and aerated, just as in a real human lymph node.
Another technological improvement was announced by ADC Biotechnology Ltd in February. The company has patents (WO2012/140433) and patent applications (WO2014/174316, WO2016/005744, WO2016/067013, and WO 2016/067016) on a novel downstream bioconjugation method expected to save 25% of total costs in ADC (antibody drug conjugate) manufacturing. In contrast to the existing approaches – which undertake bioconjugation after both the mAb/targeting moiety and cytotoxic payload have been manufactured – the new approach moves the conjugation step into the later stages of the downstream processing (DSP), with conjugation and antibody purification carried out concurrently by binding them to a resin. The drug conjugate field got a boost in February when ADC heavyweight Seattle Genetics licensed Pieris’ antibody-like anticalins for US$1.2bn. In February, Spanish PharmaMar started its own business that identifies structural diversity from sea organisms and resynthesizes novel toxic payloads for ADCs and anticalinDCs.


 Unsplash+
Unsplash+
 Bayer AG
Bayer AG