Immunooncology: Roche presents blood biomarker test
Roche is trying to offer a solution for patient selection in immunooncology. At the ESMO congress in Madrid, the theranostics company presented a liquid biopsy test that measures the tumour mutational burden in order to predict the probability for response to immunotherapy.
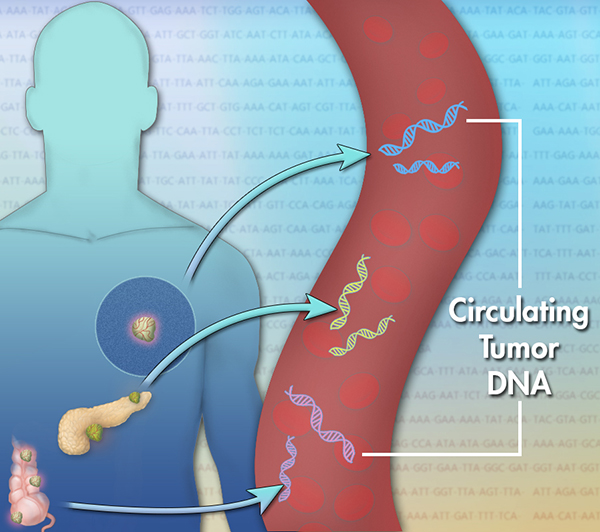
Two years ago, US researchers found a statistical correlation between response to Merck &Co’s PD1 checkpoint inhibitor pembrolizumab and the number of cancer-related mutations. Building on these findings, Roche and Foundation Medicine Inc, in which Roche holds a majority stake (56.3%), developed a a blood-based test that measures tumour mutational burden (TMB), the number of mutations within a tumour genome. In contrast to tissue biopsies such liquid biopsy assays are less invasive and, theoretically, could be used to monitor biomarkers predictive for prognosis, thus delivering therapy decision support. As TMB has been found to be an indicator of likelihood of progression-free survival (PFS) benefit from pembrolizumab monotherapy in patients with non-small cell lung cancer (NSCLC) Roche suggested that its blood-based TMB test may help to personalise cancer immunotherapies.
Pursuing next generation biomarker development is a critical component of our cancer immunotherapy strategy, said Sandra Horning, MD, Roche’s Chief Medical Officer and Head of Global Product Development. Biomarkers will not only improve our understanding of immune biology but will ultimately help match our therapies and combinations to the people most likely to benefit. This blood-based TMB assay is one example of how we and our partners are advancing the science toward personalisation of cancer therapy.
The bTMB biomarker study being presented at ESMO was conducted using 794 plasma samples from the pivotal Phase II POPLAR and Phase III OAK Tecentriq studies, in which Roche investigates safety and efficacy of its PD-L1 blocker atezolizumab. The purpose of the analysis was to collect retrospective evidence of an association between bTMB and atezolizumab activity. In the phase II POPLAR and phase III OAK clinical trials, Roche found that patients with NSCLC and high TMB experienced longer progression-free survival when treated with atezolizumab. The biomarker evaluable population (BEP) included 211 patients in POPLAR (ITT population=287) and 583 patients in OAK (excludes patients with known EGFR/ALK mutations; ITT=850), with blood samples available for targeted genomic sequencing.
To provide a proof of concept, however prospective studies are the current gold standard. Accordingly, a semi-prospective and a prospective study in patients receiving first-line treatment for NSCLC are underway, which aim to clinically evaluate and prospectively validate Roche’s blood-based diagnostic assay and assess the efficacy and safety Tecentriq (atezolizumab) and/or Alecensa (alectinib) for patients with NSCLC.
The B-F1RST study is a single-arm study evaluating the safety and efficacy of Tecentriq in first-line NSCLC and will evaluate the association between bTMB and efficacy in biomarker-unselected patients through prospective collection of blood samples that will be retrospectively tested.
BFAST is a Phase II/III trial designed to evaluate the safety and efficacy of Tecentriq or Alecensa in patients with unresectable, advanced or metastatic NSCLC. Treatment selection of Tecentriq or Alecensa is based on the presence of a positive bTMB score or oncogenic somatic mutations, respectively.
Though PD1- and PD-L1 checkpoint inhibitors have shown huge benefit to patients with inflamed tumour phenotype, the drug class currently is subject to FDA review. After placing a full hold on two trials in which Merck &Co.’s PD1 blocker pembrolizumab + chemotherapy led to a disproportionate number of deaths in patients with multiple myeloma, the Agency put partial holds on other clinical trials involving six studies with AstraZenecas PD_L1 blocker Infinzi (durvalumab) plus immunomodulatory agents developed by Celgene and three trials involving BristolMyers Squibbs PD-1 inhibitor Opdivo (nivolumab) in combination therapies though there were no unexpected safety signals.



 Boehringer Ingelheim
Boehringer Ingelheim Olga Yastremska, New Africa, freepik
Olga Yastremska, New Africa, freepik