TB urine test outperforms standard of care
A new, non-invasive tuberculosis urine test prevents common disadvantages of the standard tuberculin skin test: Measuring lipoarabinomannan glycan from M. tuberculosis, it detects the active disease in early stage and does not interfere with co-infections or weakened immune system.
Until today, it was not possible to differentiate latent from active infection with Mycobacterium tuberculosis, the pathogen that causes tuberculosis (TB) in 9.6 million people annually. Additionally, the indirect tuberculin skin test, which identifies antibodies against the pathogen by injection of bacterial proteins subcutaneously, cross-reacted with other microbioal pathogens resulting in false-positive diagnoses. Furthermore, the current standard-of-care delivered false-negative results in immunocompromised and young people. The novel urine test, developed by a research team from the US, Italy, Peru, and the UK, prevents these inaccuracies by directly measuring a mycobacterial glycan. The researchers headed by Alessandra Luccini from George Mason University say the technology presented in Science Translational Medicine will have broad implications for screening, transmission control, and treatment management, particularly because it allows testing in low-resource settings because samples can be collected noninvasively and without specialised training. "A rapid test could help millions of people worldwide", said Luccini.
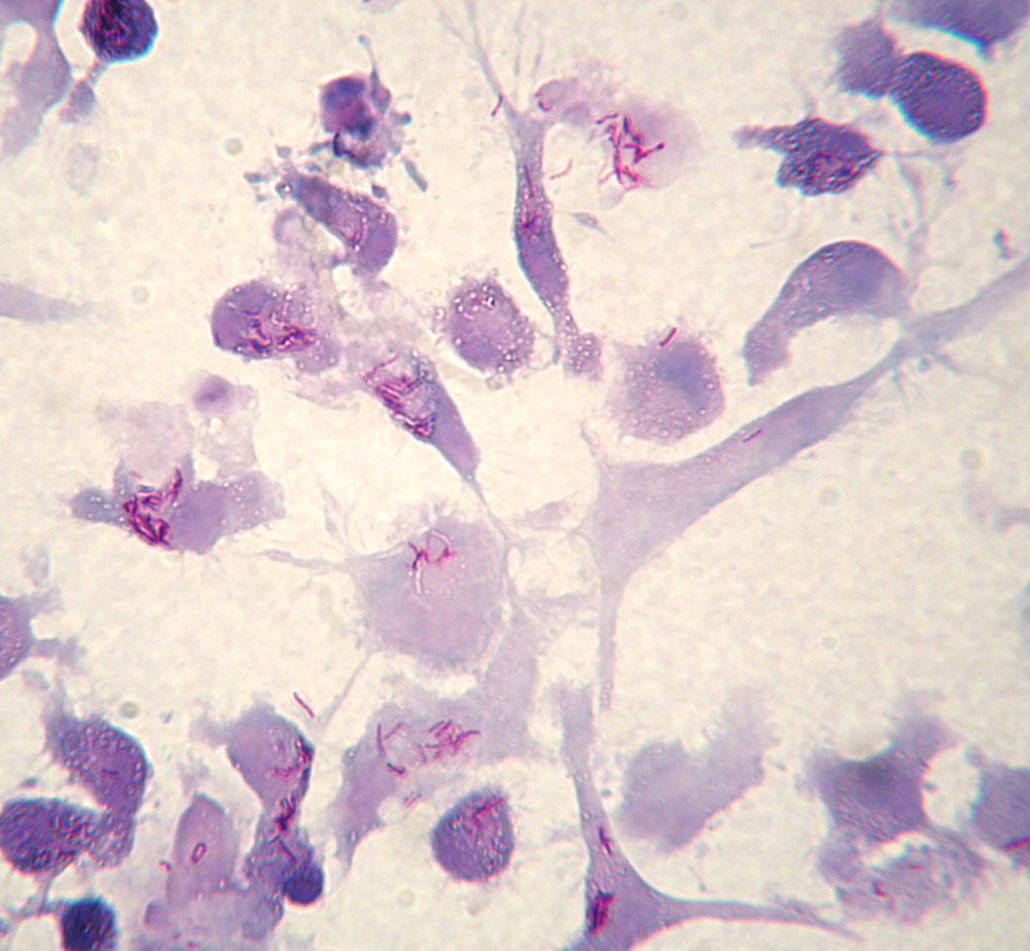
Tuberculosis is one of the most deadly bacterial infections, with 1.5 million deaths reported worldwide in 2014. Previous attempts to develop urine tests for TB have only detected infections in HIV-positive patients, possibly because the HIV-triggered immune suppression leads to substantially elevated bacteria levels in the body. Seeking to capture small amounts of a sugar called lipoarabinomannan (LAM) from the TB pathogen’s outer coat in urine, first author Luisa Paris and colleagues screened 37 compounds to narrow in on a copper complex dye called RB221 that they embedded in nanocages, tiny hydrogel meshes. Nanocages could also be used to detect cytokines and other antigens present in low concentrations in urine, demonstrating the versatility of the technology as a method to detect and monitor infections.
The RB221 nanocages trapped LAM from urine, increasing detection sensitivity by 100- to 1,000 fold, all while excluding interfering compounds from the samples that could confound results. In 48 Peruvian HIV-negative tuberculosis patients who hadn’t yet been treated, the new test detected infections with more than 95% sensitivity. What’s more, LAM levels seem to reflect the pathogen load/disease stage: elevated LAM concentrations in urine correlated with increased amounts of bacteria and more severe disease as measured by weight loss or cough.
The researchers also created nanocages to trap and detect other hallmarks of infection including very low abundance molecules named ESAT6 and CFP10. According to the authors, their next steps are to compare urinary LAM in patients before and after therapy to evaluate potential treatment-induced changes. Besides monitoring treatment efficacy, the new test has the potential to identify early stage disease even in young and old people, in which the TST often failed to deliver proper results. It can also distinguish active from latent infections, and thus prevent TB spread. Specifity of the test (currently 80%), however, has to be improved, because it can be applied broadly. However, eight of nine patients who were smear-negative and culture-positive for TB tested positive for urinary LAM.


 Bayer AG
Bayer AG
 Picture from Ferdinand Stöhr on Unsplash
Picture from Ferdinand Stöhr on Unsplash