Researchers report how body fat affects imune cells
US scientists have found that the complex interactions between fat tissue and the immune system are mediated by interleukin 33 (IL-33).
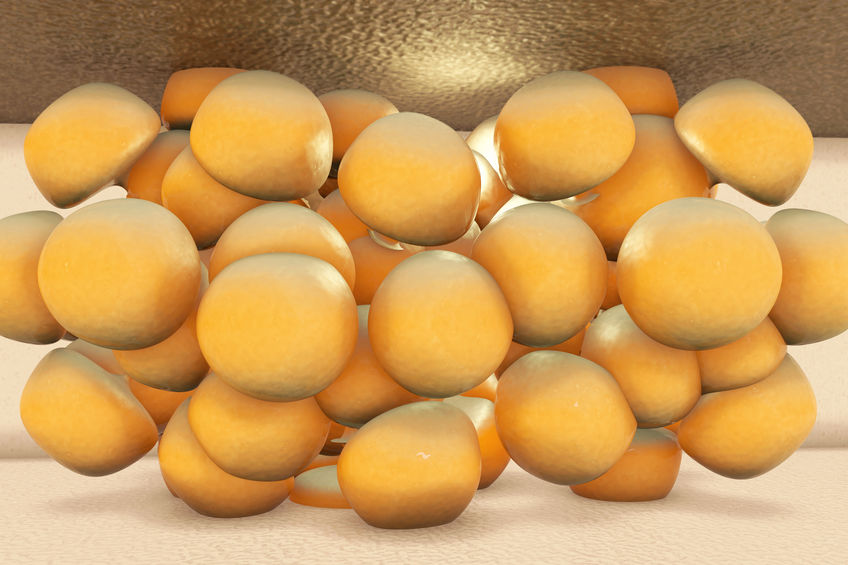
While the initial discovery of the presence of immune cells in fat was a surprising revelation to the field of immunology, it is now well-known that dysregulation of immune cell activity in white fat – one source of the body’s energy reserves – can lead to local inflammation, type 2 diabetes and obesity. IL-33 sustains a unique population of immune cells in fat tissue, including T regulatory cells (Tregs), which tamp down inflammation, but the true identity of fat-residing cells that produce IL-33 remained unclear.
Using single-cell RNA sequencing on cells from mice of different ages, sexes and disease states, Raul German Spallanzani and colleagues defined five distinct subtypes of mesenchymal stromal cells (mSCs) that can differentiate into many different cell lineages, including three subtypes that produce IL-33.
Exposing 14-week-old male mice to a high-fat diet for four to 16 weeks, the scientists found metabolic abnormalities were accompanied by a reduction in fat tissue Tregs and in IL-33-expressing mSCs. Interestingly, by 16 weeks, mSCs rebounded to higher-than-normal levels (though Treg levels stayed low), suggesting that obesity breaks down the correlation between Tregs and mSCs, possibly because a high-fat diet compromised Treg numbers – preventing them from keeping IL-33-expresssing mSCs in check.
In another study, Tanel Mahlakõiv et al. identified two sources of IL-33 in white fat: mesothelial cells, a cell population that forms a protective layer over organs in abdominal, lung and heart cavities, and adipose stem and progenitor cells (ASPCs), mesenchymal precursor cells that have the potential to give rise to multiple fat cell types. The researchers found ASPC-derived IL-33 triggered a regulatory circuit that restricted the activation of inflammatory signals in white fat, helping sustain normal tissue conditions.
In IL-33-deficient mice, a high-fat diet triggered a switch toward an inflammatory state in white fat, accompanied by increased numbers of inflammation-triggering cells like macrophages and dendritic cells. Interestingly, in mice infected with parasitic worms in the abdominal cavity, mesothelium-derived IL-33 acted as an alarmin, a type of molecule inside cells that signal tissue and cell damage to the immune system.



 adobe.stock.com - ipopba
adobe.stock.com - ipopba BioDlink
BioDlink