First immunotolerant allogenic cell transplants revealed
Researchers for the first time have found a way to prevent immune rejection of allogenic iPSC-derived cell and tissue transplants.
Though induced pluripotent stem cells (iPSCs) provide a cell source that propagates unlimited and can be differentiated in any tissue of the body, they couldn’t be used in acute organ repair strategies because the generation, differentiation and proliferation of patient-derived (autologous) iPSCs is time-consuming and laborious.
Prefabricated cell or tissue transplants from iPSC donors allogenic iPSCs), however, suffered from the vigorous immune response against histo-incompatible cells. In Nature Biotechnology, an international team of researchers headed by Sonja Schrepfer (USCF, San Francisco) and Hermann Reichenspurner (University Hospital Hamburg-Eppendorf) for the first time present a way around the problem, equipping allogenic iPSCs with an "immune-invisibility cloak" that makes them invisible for the immune system. "This is an important step on the way to the development of a universal stem cell therapy," stressed Schrepfer. "Donor organs are decreasing worldwide and organ transplantation waiting lists are getting longer and longer", added Reichenspurner. "We have great need for alternative therapeutic strategies for patients with organ failure. One promising strategy is cell therapy, which replaces organs or tissues with new stem cell-derived cells. " According to first author Tobias Deuse, this is the first time anyone has engineered cells that can be universally transplanted and can survive in immunocompetent recipients without eliciting an immune response.
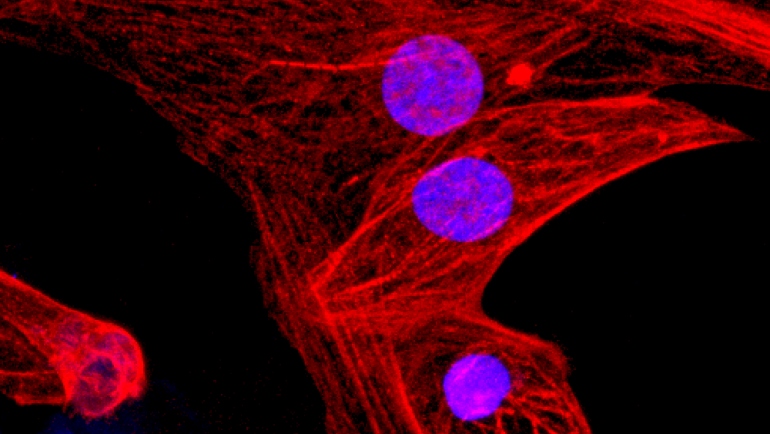
The researchers overexpressed the CD47 molecule, which mediates immune tolerance for fetal cells and organs in pregnant women for fetal cells and organs by sending a do not eat me signal against cells of the innate immune system such as macrophages and NK cells, in both allogenic mouse and human IPSCs, and specifically knocked-out the major histocompatibility complex (MHC) class I and II genes, which present foreign antigens to the immune system. The resulting iPSCs were not attacked by the immune system of humanised mice. What’s more, the iPSCs retained their pluripotent stem cell potential and differentiation capacity.
Endothelial cells, smooth muscle cells, and cardiomyocytes derived from these hypoimmunogenic mouse or human iPSCs reliably evaded immune rejection in fully MHC-mismatched allogeneic recipients and survived long-term without the use of immunosuppression. According to Schrepfer, "the production of patient-derived iPS cells is very time consuming and costly. Quality controls are difficult and the generation of cells varies greatly from patient to patient." Now, researchers have an alternative: to produce universal iPS cells, engineer them to prevent immune rejection and differentiate prefabricated cell or tissue transplants for immediate use. Our technique can benefit a wider range of people with production costs that are far lower than any individualized approach", said Deuse. "We only need to manufacture our cells one time and we’re left with a product that can be applied universally.



 adobe.stock.com - ipopba
adobe.stock.com - ipopba BioDlink
BioDlink