Microbiome defines gut conditions
Differences in microbiome composition can help to distinguish inflammatory bowel disease (IBD) and irritable bowel syndrome (IBS), Dutch and US researchers report.
Studying over 1,700 individuals delivered differences in gut microbiome composition and function among patients with the inflammatory conditions. The results could help aid in the identification of new therapeutic targets, the researchers from University Medical Center Groningen and Massachusetts Institute of Technology in Cambridge believe.
IBD and IBS are two of the most common gastrointestinal disorders, affecting up to 0.5% and 21% of the population worldwide, respectively. The conditions cause healthcare costs of over $10bn annually in both the US and Europe.
So far, other research groups identified shifts in the gut microbiome that seem associated with both disorders, but few studies have fully profiled the highly individual community of gut bacteria present in IBD and IBS patients. To bridge this gap, Arnau Vich Vila et al. sequenced stool samples from 355 IBD patients, 412 IBS patients and 1,025 controls.
Statistically, they identified groups of bacteria that were associated with IBD and IBS and saw that both patient groups harboured a reduced diversity of beneficial species and an increased diversity of disease-causing species. Furthermore, bacterial growth rates were altered in nine species in IBD patients and one species in IBS patients, and both groups displayed a higher abundance of proteins associated with antibiotic resistance.
The researchers fed their data into machine learning algorithms to create a model that could discriminate between IBD and IBS. They conclude that the results still must be validated in larger populations.
In another paper of the same issue, researchers from Queen Mary University of London, INSERM in Toulouse and University Bologna report they have found that the polyunsaturated fatty acid (PUFA) metabolite 5-oxoETE promotes excessive sensitivity and chronic pain in animal models of irritable bowel syndrome (IBS). Tereza Bautzova and co-workers believe targeting this molecule could potentially serve as the basis of new pain-relieving therapies.
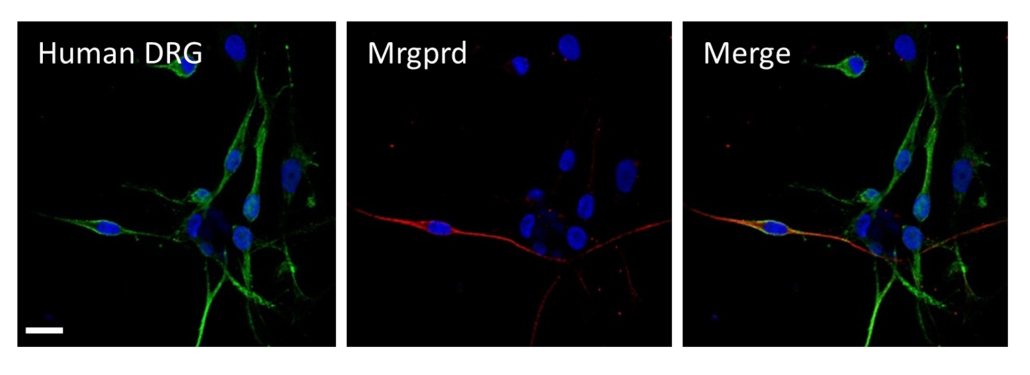
5-oxoETE induced sensitivity to pain when locally administered to mice, and stimulated the activation of isolated, pain-sensing mouse neurons. When the authors treated human sensory neurons with 5-oxoETE, they found the compound stimulated the neurons through a molecular pathway mediated by a receptor named Mrgprd (see photo). Neurons from mice deficient in Mrgprd were less likely to respond to 5-oxoETE and were less sensitive to pain, hinting that this receptor plays a critical role in IBS-associated pain sensitivity.


 Sitryx Therapeutics
Sitryx Therapeutics
