Biomarker identifies high-risk COVID-19 patients
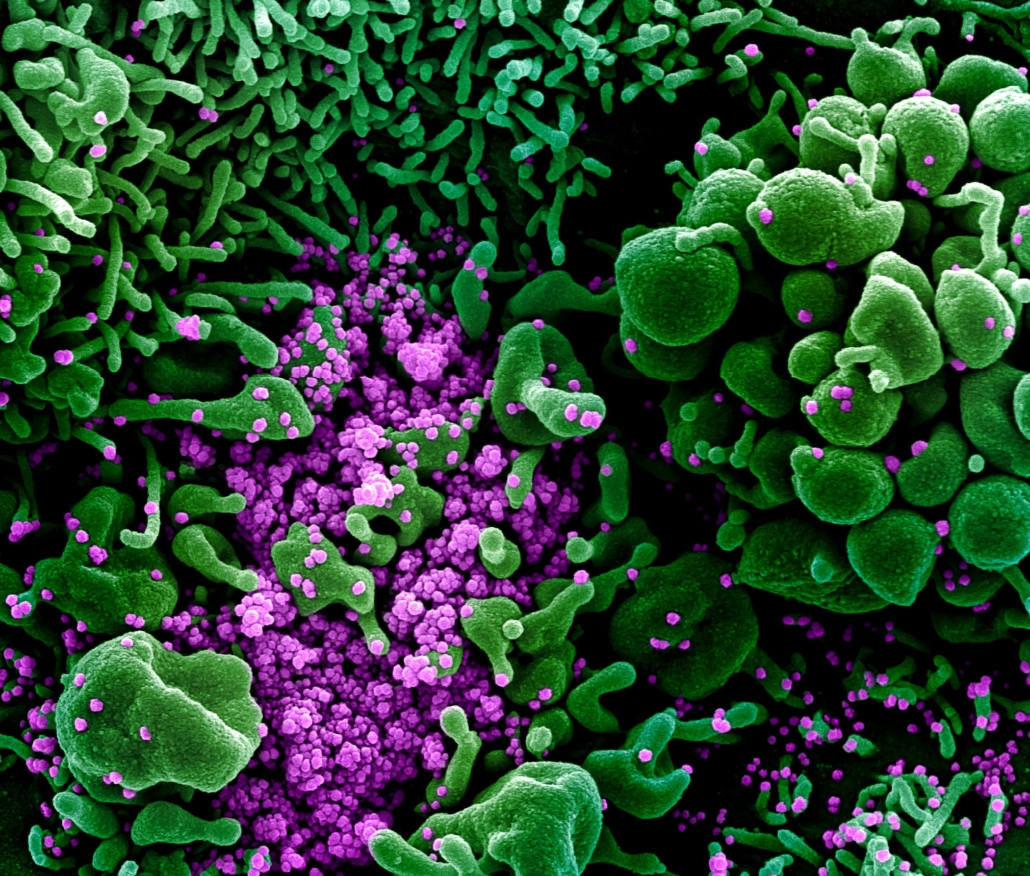
Austrian researchers have found that a lack of activation of the NK receptor is highly associated with severe COVID-19 disease courses.
On their surface, NK cells have special, activating receptors, including the NKG2C receptor, which communicates with a virally infected cell via one of its specialised surface structures, HLA-E. This interaction results in the destruction of virus-infected cells. However, due to a genetic variation, approximately 4% of the population naturally lack the activation receptor NKG2C, and in 30% of the population this receptor is only partially available.
In Genetics in Medicine, the virologists reported that people who required hospitalisation with COVID-19 were significantly more likely to exhibit the genetic variation in the KLRC2 gene underlying the lack of the receptor than people who only experienced mild disease. According to Puchhammer-Stöckl, "absence of the receptor was particularly prevalent in COVID-19 patients being treated in intensive care units, irrespective of age or gender. Genetic variations on the HLA-E of the infected cell were also associated with disease severity, albeit to a lesser extent."
Investigating the distribution of KLRC2 deletion and HLA-E*0101/0103 allelic variants in a study cohort of 361 patients with either mild (N?=?92) or severe (N?=?269) COVID-19, the researchers demonstrated that the KLRC2del, and at a lower degree the HLA-E*0101, allele were significantly overrepresented in hospitalized patients (p?=?0.0006 and p?=?0.01), particularly in patients requiring intensive care (p?<?0.0001 and p?=?0.01), compared with patients with mild symptoms. Both genetic variants were independent risk factors for severe COVID-19.
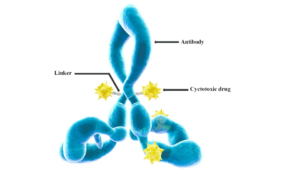
Currently, there is only one treatment (dexamethasone) available that significantly reduces mortality in late stage patients. However, virus-neutralising antibodies such as the FDA-approved REGN-COV antibody mix developed by Regeneron may be administered directly after COVID-19 diagnosis to high-risk patients. As Regeneron currently suffers from a lack of production capacities and mutations might reduce efficacy of first-generation monoclonal antibody therapeutics, European drug developers have urged EU governments to put significant amounts of money into the development of antivirals to broaden the therapeutic portfolio for doctors and to reduce the number of infected people dying from COVID-19.


 International Journal of Molecular Sciences, doi: 10.3390/ijms17040561 JO - s
International Journal of Molecular Sciences, doi: 10.3390/ijms17040561 JO - s
 Roche
Roche