Bioprinting: Screening drugs in multiple dimensions
90% of all preclinical drug candidates fail to make the grade. Now novel methods that employ miniaturised organs could help overcome this healthcare hurdle. Researchers and CROs are testing a range of models - whether grown from stem cells or spit out by 3D bioprinters - to identify toxicities, simulate cancer development and identify responders to expensive therapies. The field of 3D microtissue-based screening is just a decade old, but it clearly is soon going to play a key role when it comes to improving productivity in drug development.
According to Jürgen Knoblich from the Institute of Molecular Biotechnology (IMBA) in Vienna – a sister institute of Boehringer Ingelheim-funded IMP – it’s just a matter of time before three-dimensional miniature organs will play a significant role in drug development. We’ll see applications of organoids very soon, starting in toxicology screening, said the institute’s Deputy Scientific Director in mid-October. He was speaking at the first international meeting of experts in the field of Organoids: Modelling Organ Development and Disease in 3D Culture, an event that took place at the European Molecular Biology Laboratory (EMBL) in Heidelberg.
Many experts are convinced that multicellular in vitro 3D disease models more properly replicate the complex biology observed in the human body than 2D cell monolayers ever could. At the moment, the latter are currently used for drug screening, but often deliver results that can’t be reproduced in costly in-man clinical trials. Evidence is growing increasingly clear that tumour behaviour is the result of a finely tuned interaction of cancerous cells with surrounding fibroblasts, invading immune cells and vasculature. And that is only reflected by 3D models, explains cancer-cell culture expert Helmut Dolznig from Vienna Medical University. Knoblich agrees: Organoids have already delivered models for different cancers, for liver diseases and for rare diseases like cystic fibrosis.
How 3D models personalise meds
Using patient-derived colon cells that self-organised into 3D-miniguts carrying a defective variant of the CTFR gene (del508), researchers at Utrecht University Medical Centre and Dutch CRO Ocello (Leiden) have already successfully quantified how well patients respond to Vertex Pharmaceuticals’ cystic fibrosis (CF) drugs Kalydeco and Lubacaftor. Unlike tests that identify the mutations underlying the rare disease, the 3D high-throughput assay developed by Johanna Dekker’s team is functional. In basic terms, it can be used to quantify how well drug candidates restore the defective calcium channel function that leads to CF symptoms in 80% of all patients. In this sense, organoid tests could add a whole new quality dimension to personalised medicine.
Big Pharma and 3D printing
In the field of 3D disease modelling, two schools of thought are having an impact at the moment. Both offer advantages and disadvantages. What can 3D models do that 2D models can’t? When we produce organoids from stem cells in the lab, says Knoblich, the cells self-organise into the functional forms, delivering both proper microarchitecture and cell types. We allow them to self-organise, and the result is functional organoids. But there’s a competing approach.
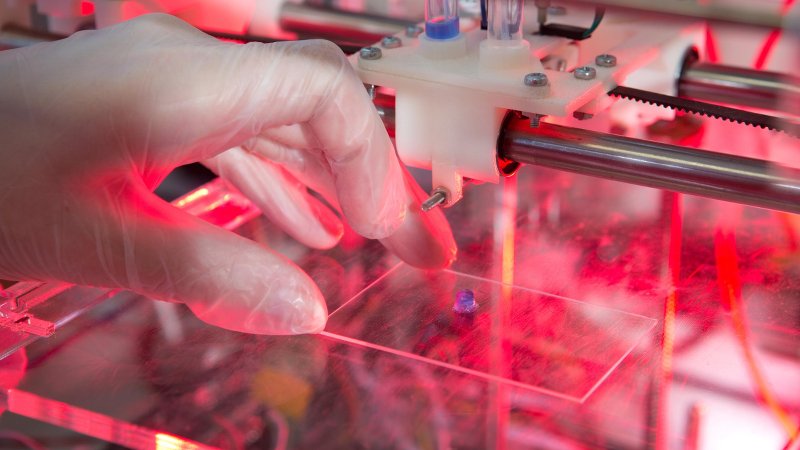
3D printers allow for automatic reproducible production of an exact copy of a tissue – including complex 3D architecture, biochemical gradients and combinations of cells and vasculature like those found in a functional liver or placenta, says Lutz Kloke, who founded Berlin-based Cellbricks last year. His firm has developed a novel bioprinter, and established ten partnerships to develop specific microtissues for R&D, as well as for the fields of drug development and tissue engineering.
Read the full background on 3D Bioprinting in our print magazine!


 ©FabienMalot
©FabienMalot Lonza Group
Lonza Group Vetter Pharma
Vetter Pharma