Cell-based vaccination vs mortality-reducing therapies
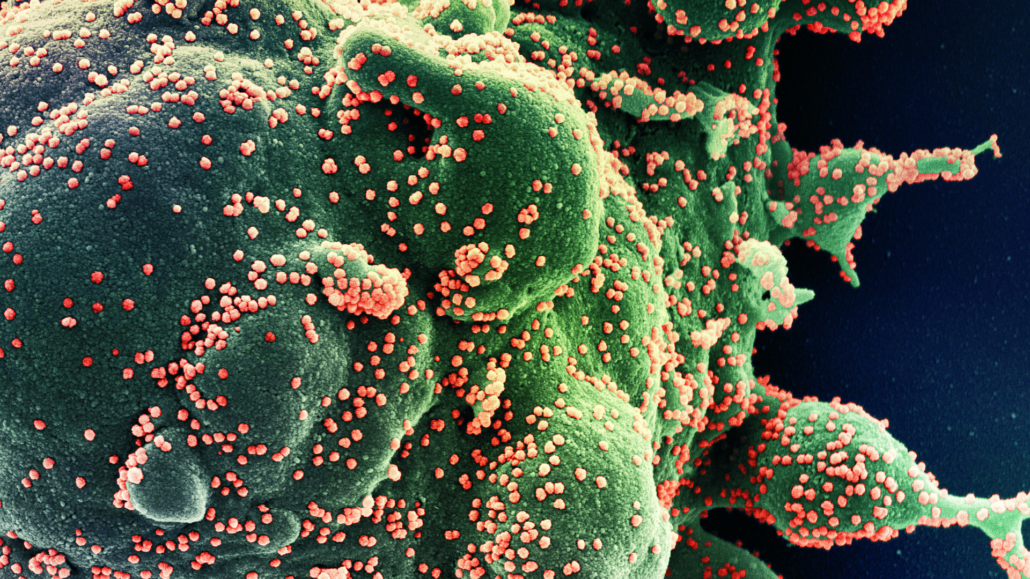
Immunovative Therapies Ltd and its US subsidiary Mirror Biologics Inc. are testing a novel, T cell-based vaccination concept that might protect risk groups from new SARS-CoV-2 variants and any emerging viral pandemic in the future. However, therapies that significantly reduce the mortality rate of COVID-19 patients may be a cheaper way compared to vaccines to protect high-risk groups. UK researchers reported on the first therapy in mid-June.
In contrast to classical vaccine approaches, Immunovative’s allo-priming strategy addresses the phenomenon of viral evolution. In mid-May, for the first time, the company’s CEO Michael Har-Noy and colleagues presented a technology that might provide a universal anti-viral vaccine designed to protect immunocompromised humans and elderly adults from the current SARS-CoV-2 pandemic but also from any future novel virus outbreaks.
The vaccination concept appears more convincing than current vaccination approaches, which will last only for one year, according to AstraZeneca’s CEO Pascal Soriot. Patients will receive a series of injections of bioengineered Th1-cells, which are thought to remodel the ageing immune system to reverse immunosenescence and protect against chronic inflammation. According to CEO Har-Noy a Phase I/II clinical protocol for testing the concept in 40 healthy adults over 65 years was cleared by the US FDA at the end of June and and enrolment will start by August. We will be collecting blood from the elderly volunteers and challenging the blood with a panel of live viruses to determine if the remodelled immune system can suppress the propagation of SARS-CoV2 and influenza A and B viruses cultured on human lung endothelial cells, Har-Noy told European Biotechnology. We are currently seeking partners for EU and China and South-east Asia.
Preclinical success
According to Immunovative Therapies Ltd, allo-priming, which triggers cell-based immunity, provides a back-up in case vaccination strategies designed to elicit neutralising antibody protection fail to protect the vulnerable elderly population. Allo-priming is performed using activated, intentionally mismatched, ex vivo differentiated and expanded living Th1-like cells (AlloStim®) derived from healthy donors.
Preclinically, multiple intradermal injections of AlloStim® created a dominant titer of allo-specific Th1/CD8-T-cytotoxic memory cells in circulation, replacing the dominance of exhausted memory cells of the aged immune system. Upon viral encounter, bystander activation of the allo-specific memory cells caused an immediate release of interferon gamma (IFN-g), stopping viral transcription and leading to bystander activation of innate, cellular effector cells and activation of cross-reactive, allo-specific, CD8-T-cytotoxic lymphocytes (T killer cells).
Mainstream vaccination approaches have not been very successful in protecting against emergent viruses, such as HIV, hepatitis C, Zika, dengue, and the pandemic SARS and MERS coronaviruses, which mutate and adapt very rapidly to their hosts.
Feeble vaccination
In contrast to childhood diseases, these vaccines will not provide lifelong protection, because they are based on an approach that ignores viral evolution, which makes sense for pathogens such as measles or other childhood diseases. For this reason, current vaccine technology platforms may not produce a timely, protective vaccine against COVID-19 and could result in a vaccine that becomes obsolete after a viral mutation. This would present a good business opportunity for vaccine makers but a lottery game for high-risk groups. Another point that is currently widely ignored: traditional vaccines could make rapidly mutating and adapting pathogens more aggressive. Under normal conditions, viral pathogens never become extremely deadly, because they can only spread effectively if most of their hosts survive the infection and are not protected by widespread or herd immunity in the target population.
Dangers and hopes
As vaccines create a selection advantage for viruses, which could enter and reproduce themselves ultra-rapidly in the host cell, they might trigger a kind of vaccine-driven evolution, eventually making
viruses more deadly and devastating as postulated for vaccine against Marek’s disease vaccines, a neoplastic disease of poultry. Michael Har-Noy said in a press release: While there is great optimism regarding current clinical trials investigating protective vaccines against COVID-19, there is a very real possibility that none of the vaccine candidates under investigation will prove to provide long-term protection from COVID-19, and some vaccine candidates may even make symptoms worse. Even in the event that an effective vaccine is timely developed, such a vaccine likely would not be as effective in providing protective immunity in the elderly. If allo-priming is proven to work as designed, a single series of shots could protect against the current pandemic as well as any future pandemic.
Cheap protection for risk groups
In mid-June, a faster and cheaper way to protect those who are at the highest risk to develop the life-threatening host immune response following the blood infection with SARS-CoV-2 was reported by researchers from the University of Oxford (UK). Within the systematic
RECOVERY study designed to test the efficacy of drugs approved in other indications, they identified dexamethasone as the first drug that reduced COVID-19 mortality in ventilated patients.
A first step but no breakthrough
News reports immediately claimed the corticoid drug dexamethasone to be a breakthrough in the fight against SARS-CoV-2. However, more effective drugs or combinations therapies might improve the likelihood of rescuing a higher percentage of ventilated patients.
According to Principal Investigator Peter Horby from the University of Oxford, the cheap immuno-modulatory drug dexamethasone helped reducing mortality by about one third in ventilated
COVID-19 patients compared to the current standard of care. That means that one death could be prevented by this treatment out of around eight ventilated patients. The clinical trial in which 2,104 COVID-19 hospitalised patients received dexamethasone for 10 days vs 4,321 patients receiving standard-of-care treatment was part of the UK’s RECOVERY (Randomised Evaluation of COVid-19 thERapY) study that systematically combines potential COVID treatments and compares them with the current standard of care. Similar systematic studies are currently being conducted in the US and Europe.
What sounded good at first sight: dexamethasone, a DMARD (Disease Modifying Anti-Rheumatic Drug) reduced deaths by one-third in ventilated COVID-19 patients and by about one fifth in other patients receiving oxygen only. There was no benefit among those patients who did not require respiratory support. Dexamethasone is the first treatment that demonstrates a survival benefit for patients in severe WHO disease stages 5 to 7. For comparison: the hyped antiviral drug remdesivir (Gilead Sciences) only helped patients with moderate symptoms but did not demonstrate any significant survival benefit (mortality rate of 7.1% vs 11.9% for placebo) in a Phase II study.
The discovery of a treatment that is widely available at a cost of only €16 per 10-day trial per patient may end protectionism of richest Western countries that tried to secure potential COVID-19 jabs to vaccinate their citizens. US President Donald Trump initiated this tragic chapter in health policy with a project called Operation Warp Speed, which is funded by the US agency BARDA and intended to give the US access to COVID-19 vaccination. Germany, Italy, the Netherlands, and France followed suit in mid-June, securing 300 million doses of an adenoviral vector vaccine licenced from the University of Oxford by AstraZeneca.
High production capacity
Even in the case of dexamethasone, the UK government stockpiled 200,000 doses of the drug. But, the good news is that enough of the corticosteroid is available on the world market to treat all those, who need mechanical ventilation about 5% of people diagnosed with SARS-CoV-2 develop severe disease symptoms. Currently, about 50% of them die. Last year, China produced 32.354 tons of the drug just in Q4/2019, sufficient for 500,000 10-day treatments.
These preliminary results from the RECOVERY trial are very clear, said Martin Landray, another investigator, dexamethasone reduces the risk of death among patients with severe respiratory complications. COVID-19 is a global disease; it is fantastic that the first treatment demonstrated to reduce mortality is one that is instantly available and affordable worldwide.
No other therapy has shown a recovery benefit until now. Still, as the drug is an immunosuppressant, it can eventually promote opportunistic infections.
This article was published in European Biotechnology Magazine Summer Edition 2020.


 ©FabienMalot
©FabienMalot Lonza Group
Lonza Group Vetter Pharma
Vetter Pharma